Author: Andrew P Volans / Editor: Tajek B Hassan / Reviewer: Andrew P Volans / Codes: AP1, AP2, AP3, DC11, GP1, MaC3, MaP2, OncC3, PhP1, RC2, RP2, SLO1, SLO3, SLO5, SuP1 / Publication Date: 22/04/2021
Context
Patients frequently attend the emergency department (ED) with episodes of cutaneous and mucosal swelling. These are routinely diagnosed as allergy and are then treated with antihistamines, steroids and adrenaline, depending on the clinicians view of the seriousness of the attack.
In a significant number of these cases, there is no apparent change in the patients condition over several hours of observation and in many cases these patients are discharged with reassurance and a course of antihistamines and steroids.
Many emergency clinicians will have seen patients with allergic airway obstruction where routine treatment with antihistamine and adrenaline has not worked and the patient has required intubation or even surgical airway, and a few will have seen patients where this intervention has failed to rescue the patient.
Over recent years there have been significant advances in the understanding of the patho-physiology of angioedema and consequently new specific therapies have evolved for non histamine mediated swellings and as a result it is important for emergency physicians to be aware of these advances [1,2].
One problem for patients with this syndrome is the perception the angioedema is a rare condition and therefore we are unlikely to see many cases in practice.
An audit of the authors department attendance recording the codes for allergy, angioedema and anaphylaxis identified 68 patients within 3 months (monthly census of 4,000 new patients). Review of the patients notes revealed 28 patients with symptoms that settled rapidly with antihistamines and 29 where the symptoms did not respond. One patient had recently diagnosed HAE. In 11 the records were too vague to make a judgement.
During the same period there were 18 diabetic keto-acidosis, 20 NSTEMI and 11 STEMI codes.
The message should be that non histamine reactions are no more rare in the ED than acute myocardial infarction.
Clinical presentations and assessment
Patients will present in a number of ways.
There are a few patients who have a known diagnosis of hereditary angioedema (HAE) with a letter from their Immunologist / dermatologist or allergy specialist giving a diagnosis and a suggested treatment regimen. Some of these patients will present with their rescue medication and will be asking for assistance in delivering care, whilst others may come requesting medication re-supply after self treatment.
The majority of diagnosed HAE patients will only present to the ED when they are suffering from severe abdominal pain or airway threatening attacks.
In our audit there was a single case of recently diagnosed HAE who had not yet had any formal advice on care.
The majority of presentations to the ED will be undifferentiated swellings in patients who have no formal diagnosis or have been told they have an allergy to some unspecified allergen.
History is paramount in discriminating the probable origin of the attack.
Allergy attacks are rapid in onset, there is generally a recognisable allergen, and will be associated with a superficial itch, a generalised rash with raised wheals, respiratory wheeze, abdominal pain and possibly hypotension. Such cases must be treated with adrenaline, antihistamine and steroids with a possible need for intravenous fluid replacement.
Non histamine mediated angioedema, develops more slowly, typically over a few hours, although lethal cases are reported, with a very short history.
Facial and pharyngeal attacks (Figs 1 and 2) are at best disfiguring, preventing the sufferer from working for several days, but they are potentially lethal with 30% of HAE affected families describing airway obstruction deaths in affected family members, often associated with simple URTI. These attacks develop over 2-3 hours but have a 40 minute acceleration phase to maximal swelling. The resolution phase then lasts for up to 48 hours during which the swelling slowly declines [3].
Fig 1: Early angioedema
Fig 2: Full hemifacial angioedema
A history should be sought of previous swellings of the periphery (Fig 3) or face and episodes of abdominal pain that may have resulted in admission and often intervention under general surgery or gynaecology, most commonly without any specific causative pathology being found. Within the HAE population, 50% of attacks are abdominal/genital and 50% are peripheral/cutaneous or orofacial.
Fig 3: Peripheral angioedema
Only 1% of attacks include the larynx, but sufferers have multiple attacks and all describe oropharyngeal symptoms during some attacks. It is such attacks that bring known HAE patients to the ED.
Specific questions about the pattern of previous attacks including abdominal pain, and family histories of similarly affected relatives will support a diagnosis of HAE.
Question the nature of the sensation in the lesion; histamine itches but the typical angioedema lesion burns or hurts as well.
Does the patient take ACE Inhibitors or have they been using NSAIDs?
Examination reveals a different morphology in the early lesion, although severe late attacks may be difficult to differentiate (picture: hemifaciall).
Fig 4: Hemifacial angioedema
The non-response to initial therapy for allergy should raise the possibility of an alternative diagnosis for the EP [4].
Allergy conditions are triggered by exposure to environmental allergens and involve interaction with immunoglobulins, either free in the plasma or attached to cells, resulting in the release of histamine from mast cells.
Histamine release causes local superficial wheals that itch. If there is generalised release then the patient can suffer abdominal pain due to mucosal swelling and obstruction, hypotension due to vessel dilatation and leakage, as well as bronchospasm and local swelling that can affect the airway. These symptoms can be reversed by the use of adrenaline and antihistamines. Steroids will suppress the immunoglobulin production and reduce the chances of recurrent allergic response.
In 1888 Osler described angioneurotic oedema where the attacks of oedema appeared to be related to a nerve root distribution and were normally unilateral, unlike the generalised rash of allergy. He felt that there was evidence that this disorder was inheritable as it ran in families.
Attacks can affect any cutaneous or mucosal surface, the skin, the face and lips, the larynx and pharynx, the gastrointestinal or genito-urinary tracts.
Angioedema is a deep dermal, submucosal or subcutaneous swelling associated with vascular leakage.
Causes
Triggers that are recognised include: direct trauma, e.g. dental work, intubation, and peripheral injuries, infections, medications such as oestrogens (HRT and oral contraceptives), non steroidal analgesics and ACE inhibitors, and stress.
Pathophysiology
HAE became defined in the 1960s when a biomarker was identified in the form of a lack of functioning C1 esterase inhibitor (C1inhib) that was transmitted as an autosomal dominant disorder [5].
Two forms of this condition were described: Type 1, making up 85% of such cases, with a pathologically low level of C1 esterase inhibitor protein, and Type 2 (15%) where the protein concentration is near normal but it lacks function. More recently the level of Complement 4 has been shown to be low during attacks [6].
Based on this work, a treatment regimen was developed, initially using fresh frozen plasma to replace the missing factor. This has now been refined to deliver the isolated plasma derived inhibitor (Berinert, a concentrate) or (Cinryze, a nano-filtered concentrate) or more recently a recombinant inhibitor (Ruconest [1,2,7,8].
These traditional HAE types only make up about 1-2% of all cases of angioedema that present clinically. The vast majority of cases have normal levels and activities of plasma inhibitor when measured during attacks, and so another precipitating pathology needs to be sought.
More recently a new type of HAE has been described which is still being delineated. It is most commonly seen in women but not exclusively so, and it seems to be oestrogen driven and is seen to run in families. Clinically, its presentation is indistinguishable from traditional HAE other than having a normal C1inhib level and activity and a normal C4.
So far about 20% of these cases have been found to have an abnormal structural form of factor XII but how this abnormality alters its function is as yet unclear. It is also known that oestrogen up regulates both normal and abnormal factor XII activity [9,10].
Other known causes of normal inhibitor angioedema are those patients on ACE inhibitors (ACEI), where up to 2% of users can suffer from angioedema predominately affecting the lips and oropharynx. Given the incidence of ACE inhibitors in the community, this group will make up a significant number of cases that will present to the ED. The blood pressure reduction activity of ACE inhibitors is known to be related to its ability to raise bradykinin levels in the vascular bed causing vessel dilatation. The activity of angiotensin converting enzyme is known to vary between individuals. This might suggest that a patient with a low activity ACE might be more susceptible to ACE inhibitor associated angioedema [11].
In all of these defined groups of angioedema the serum level of bradykinin is found to be significantly elevated during attacks.
Other known causes are autoimmune diseases and haematological malignancies such as lymphoma. It has been shown [12] that factor XII is directly activated by contact with unfolded proteins such as Bence Jones and amyloid and it is known that factor XII is implicated in the formation of bradykinin in vivo suggesting a reason why these diseases may predispose to angioedema.
Another route to trigger angioedema is suggested by the fact that some cases of HAE type 1 develop the ability to rapidly denature the exogenous C1inhib by raising antibodies to the protein, consequently an autoimmune disease developing antibodies to C1inhib might be expected to exacerbate angioedema.
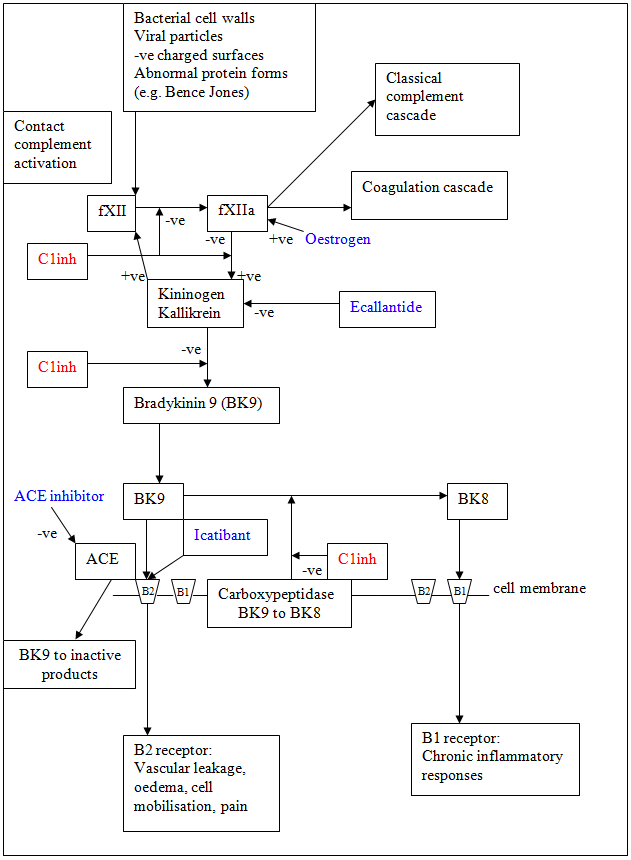
Bradykinin pathway
Bradykinin production (Fig 5) is part of the normal inflammatory process of the body. A typical and common example of bradykinin activity is the congestion of the upper airway present during an URTI.
Fig 5: Bradykinin production pathway
Factor XII
Bradykinin is generated on the surface membrane of most endothelial cells by the interaction of kallikrein and high molecular weight kininogen that circulate bound together in the plasma. Activated factor XII converts pre-kallikrein into kallikrein, which produces bradykinin from kininogen. Kallikrein also activates factor XII, driving a positive feedback [12].
Factor XII activation is part of the contact activation response of the complement cascade. The activating entity is a negatively charged surface.
In vivo this might be a viral or bacterial surface coat, or various altered proteins such as amyloid or Bence Jones protein as well as articular cartilage, endotoxins and heparin amongst other physiological auto-activation triggers.
In the laboratory, factor XII can be triggered by kaolin (e.g. the KCCT coagulation test) or glass and is the reason blood coagulates on contact with glass. Activated factor XII activates factor XI in coagulation cascade, resulting in thrombin formation.
Activated factor XII is also cleaved by kallikrein to produce another active form that activates the first step of the classical complement cascade (C1 esterase). Kallikrein also activates complement factors 3 and 5 directly, further driving the classical complement system.
Recent studies suggest that these different pathways can be triggered selectively although how this occurs is currently unknown.
The activated kininogen cleaves kallikrein to produce the 9-peptide transmitter bradykinin.
It appears that factor XII also acts as a physical anchor for the kallikrein / kininogen complex, bringing it into close proximity with the membrane bound bradykinin receptor complexes (bradykinin 1 (BK1) and bradykinin 2 (BK2)).
Bradykinin receptors
The 9-peptide bradykinin binds to the BK2 receptor where it initiates a rapid signal resulting in increased cell permeability and fluid translocation causing local cellular oedema and increased vascular leakage. It also triggers the prostaglandin cascades associated with inflammation and attracting leucocytes to the area. The BK2 activity is terminated by the bradykinin molecule being cleaved by two peptidases in close proximity to the BK2 receptor, one, ACE breaks the peptide into non active fragments, whereas a second (C1 esterase), a carboxypeptidase, within the BK1/2 complex, produces an 8 peptide BK molecule that no longer binds with the BK2 receptor but is recognised by the adjacent BK1 receptor, triggering another interaction that involves the activated BK1 complex being endocytosed resulting in the triggering of slower DNA / RNA mediated cellular changes.
Pathway controls
These activities are moderated by a number of suppressing factors.
The kininogen and carboxypeptidase activity and factor XII activation is suppressed by C1 esterase inhibitor (C1inhib) that circulates in the plasma, and as previously described, bradykinin is also broken down to non active moieties by ACE which is in close proximity to the BK2 receptor.
From this physiology, many forms of angioedema appear to be disorders of bradykinin metabolism, attacks being generated by an imbalance between production and degradation with over production of the mediator due to lack of the C1 inhib function or by an overactive or over stimulated factor XII, or reduced degradation due to an overpowering or reduction in the function of ACE.
Acutely, clinical examination and assessment are the mainstays of diagnosis. In airway compromise, the ability to view the supraglottic area and cords would assist rational planning if intubation is considered.
Routine blood testing is unhelpful, most patients showing no helpful diagnostic findings although the D Dimer level may be raised due to the cross activation of the coagulation cascade by activated factor XII.
For long term diagnosis, blood taken for C1 esterase inhibitor level and activity and C4 level during the attack, can identify those cases of HAE and be of assistance to immunologists in planning long term care [2].
The traditional treatments we, in the ED, routinely use when an airway appears compromised by swelling are adrenaline, antihistamines and steroids.
Review of the pathophysiology above suggests that steroids and antihistamines are unlikely to be effective. Adrenaline might be expected to be helpful, however experience suggests that the effect is quite small in practice.
A recent publication by the World Allergy Organisation (WAO) [2] has presented evidence-based guidelines with a number of graded recommendations.
Specific therapies
The traditional treatment for HAE types 1 and 2 was the replacement of C1 esterase inhibitor by infusion of fresh frozen plasma (FFP) with the potential infection risks of harvested plasma products and the allergy potential of exogenous proteins. Solvent detergent-treated plasma (SDP) is preferred as it confers a lower risk unless a safe supply of FFP is available.
Consequently this treatment has been downgraded by the WAO to a back up when specific therapies are not available.
Concentrations of plasma and recombinant derived C1 inhibitor are now commercially available (Cinryze (1000 U slowly iv), Berinert (20 U/Kg slowly iv) or a recombinant, Ruconest (50 U/Kg iv) and are recommended by the World Allergy Association as an initial treatment of HAE attacks with grade A evidence supporting the recommendation. Initial symptom resolution is seen after about 20 minutes with full resolution by a median of about 5 hours.
A kallikrein inhibitor (ecallantide 30 mg sc) is available in the USA but not in Europe, due to its efficacy and side effect profile.
Since the end organ mediator for angioedema appears to be bradykinin in at least four patient types, it would seem logical to consider attempting blockade of the bradykinin receptor. Currently there is a BK2 receptor blocker (Icatibant, 30 mg sc) in the formulary, which has a license for use in hereditary angioedema [13,14]. Studies and case reports also exist supporting its use in ACEI associated angioedema [11,15,16,17].
Initial symptom relief is reported at 20 minutes after injection with full symptom resolution at a median of 5 hours.
Recent Controlled trials [18,19] of Icatibant in ACEI angioedema have shown contradictory evidence concerning its effectiveness.
Studies from clinics specialising in Hereditary Angioedema, suggest that speed of drug administration is important and patients who get treatment early in the evolution of their attack can terminate their symptoms and obtain a rapid regression of symptoms and signs. Those where their rescue medication is delayed beyond 4 hours after symptom onset are forced to suffer a slow recovery that differs little from that in placebo groups in RCT’s.[20]
Given that this acts as a competitive blocker, recent studies show that the speed of resolution is faster if given early in an attack before the secondary slow receptor activation [14].
Currently, the WAO recommends that patients with known HAE be supplied with either or both these treatment modalities for use on demand to terminate attacks [2,8].
Fig 6: Current drug treatments
Tranexamic acid has been used for decades as prophylaxis for HAE with some reduction in attack frequency and consequently has been used in the acute event although studies suggest a slow response to treatment with 20+ hours before resolution. It is suggested that tranexamic acid works on the secondary prostaglandin activation.
Androgenic steroids have been a traditional treatment as prophylaxis. It has become apparent that where oestrogens increase the amount and activity of factor XII, androgens reduce both the oestrogen level and consequently the stimulation to the factor XII, and also may have a direct suppression effect on factor XII. The side effects of danozol and stanozolol limit their acceptability as prophylaxis in many patients.
Angioedema tends to recur in susceptible patients. The identification of patients with HAE and the subsequent identification of other sufferers within their family is a major role for clinicians who manage these cases in the long term. Sudden death secondary to laryngeal obstruction is relatively common within affected families and the current management strategy is to provide specific therapeutic agents that can be used on demand to terminate attacks when the patient feels that to be necessary [2,8].
To assist in identifying the type of angioedema, a detailed history of the attack pattern, the details of family history and any identifiable trigger such as drug or specific food exposure (salicylates) may help in diagnosis.
The use of ACE inhibitors associated with the attack is also important. The attack can occur at any time after first exposure to the medication to several years after regular unremarkable use. It is known that there is a significant variance in activity of ACE between patients. It therefore may be that a patient with low activity ACE will be safe from attack in normal circumstances but may become symptomatic if there is a challenge to their contact activation system increasing the level of bradykinin production. Such an event may describe a recent presentation where a patient with 6 years unremarkable exposure to ACEI developed a lower lip and tongue angioedema 48 hours after her flu vaccination.
In such cases the removal of the ACEI from her medication is probably all that is required to prevent further attacks although the time scale of resolution of the hypersensitivity is unknown.
The evidence from the use of icatibant in HAE patients reports a 1% second injection rate but at a median of 24 hours after the initial injection and it is believed to be related to a second attack rather than a failure of the first rescue medication. Similar relapse rates are seen with C1 esterase inhibitor replacement.
Traditional therapies with tranexamic acid normally see a 24 to 72 hour resolution of symptoms which match the untreated time course of the attacks.
- At presentation it is appropriate to treat initially for anaphylaxis since this is equally common and probably more rapidly fatal.
- Patients with acute airway compromise due to angioedema are in need of highly skilled anaesthetic and ENT support.
- The difficult airway kit should be on hand and retronasal endoscopy should also be available.
- Deaths or serious hypoxic complications are associated with failure to recognise the potential difficulty of the airway management. In orofacial attacks, the facial tissues are stiff and swollen and the supraglottic and glottic areas are very congested making access to the larynx very difficult. It is said by those with experience of these attacks that the nasopharynx is less affected and may offer an easier route of approach to the larynx than the oral route (personal communication).
- Patients known to have this problem will often approach an ED with early symptoms and a letter from their specialist, the importance of which can be missed by junior or ill informed staff. The patient has presented early because they are aware of their prodromes and may have learnt to recognise a potentially serious attack whilst there is little to see or record during routine clinical assessment. To ignore such cases can be fatal if the attack closes the airway during the pathognemonic acceleration phase.
- There is increasing evidence that the effectiveness of the specific medications is time limited in that their effect is to prevent progression of swelling. Once swelling has occurred, they do not speed up resolution. Consequently, they should be given whilst the swelling is actively developing and not once it has become fixed.
Currently the C1 esterase inhibitor is marketed at about £600 per vial with a standard dose being 3 vials for most adults.
The bradykinin 2 blocker markets at £1500 per syringe with a standard dose being a single syringe.
Such prices tend to cause problems for some departments with their drug committees. However, a single day on a ventilator in ITU is normally costed at between 3000 and 6000 and most cases will spend 3 or more days before extubation.
Acknowledgement
The author would like to thank his wife for the use of the clinical photos in this session.
- Maurer,M.,Magerl,M.,Ansotegui,I. et al. The International WAO/EAACI guideline for the management of hereditary angioedema-the 2017 revision and update. World Allergy Organ j 11, 5 (2018). Hyyps://doi.org/10.1186/s40413-017-0180-1
- Craig T, Ayg ren-P rs n E, Bork K et al. WAO Guideline for the Management of Hereditary Angioedema. World Allergy Organ J. 2012 Dec;5(12):182-99.
- Agostoni A, Ayg ren-P rs n E, Binkley KE et al. Hereditary and acquired angioedema: problems and progress: proceedings of the third C1 esterase inhibitor deficiency workshop and beyond. J Allergy Clin Immunol 2004:114(3):51-131.
- JaiganeshT, WieseM, HollingsworthJ et al. Acute angioedema: recognition and management in the emergency department. Eur J Emerg Med 2013;20(1):10-17.
- Donaldson VH, Evans RR. A biochemical abnormality in hereditary angioneurotic edema: absence of serum inhibitor of C 1-esterase. Am J Med 1963;35:37-44.
- Cugno M, Nussberger J, Cicardi M et al. Bradykinin and the pathophysiology of angioedema. Int Immunopharmacol 2003;3(3):311-317.
- Bowen et al. 2010 International consensus algorithm for the diagnosis, therapy and management of hereditary angioedema. Allergy Asthma Clin Immunol 2010;6:24.
- Tourangeau LM, Castaldo AJ, Davis DK et al. Safety and efficacy of physician-supervised self-managed C1 inhibitor replacement therapy. Int Arch Allergy Immunol 2012;157:417-424.
- Binkley KE. Factor XII mutations, estrogen-dependent inherited angioedema, and related conditions. Allergy Asthma Clin Immunol 2010;6:16.
- Bernstein JA, Moellman J. Emerging concepts in the diagnosis and treatment of patients with undifferentiated angioedema. Int J Emerg Med 2012;5:39.
- Molinaro G, Cugno M, Perez M et al. Angiotensin-converting enzyme inhibitor-associated angioedema is characterized by a slower degradation of des-arginine9-bradykinin. JPET 2002;303:232-237.
- Schmaier AH. The elusive physiologic role of Factor XII. J Clin Invest 2008;118(9):3006-3009.
- Bork K, Frank J, Grundt B et al. Treatment of acute edema attacks in hereditary angioedema with a bradykinin receptor-2 antagonist (Icatibant). J Allergy Clin Immunol 2007;119(6):1497-1503.
- Maurer M, Aberer W, Bouillet L et al. Hereditary angioedema attacks resolve faster and are shorter after early icatibant treatment. PLoS ONE 2013;8(2).
- Volans A, Ferguson R. Using a bradykinin blocker in ACE inhibitor-associated angioedema in the emergency department. BMJ Case Reports, 2013.
- Bas M, Greve J, Stelter K et al. Therapeutic efficacy of icatibant in angioedema induced by angiotensin-converting enzyme inhibitors: a case series. Ann Emerg Med 2010;56(3):278-282.
- Bruce L. Zuraw, Konrad Bork, Karen Binkley, et al. Hereditary angioedema with normal C1 inhibitor function: Consensus of an international expert panel. Allergy Asthma Proc. 33:S145-S156, 2012; doi:10.2500/aap.2012.33.3627
- Murat Bas, Jens Greve, Klaus Stelter et al. A Randomized Trial of Icatibant in ACE-Inhibitor Induced Angioedema. N Engl J Med 2015: 372:418-425. doi:10.1056/NEJMoa1312524
- Brittany T Straka, Claudia E Ramirez, James B Byrd et al. Effect of Bradykinin receptor antagonism on ACE inhibitor associated angioedema. J Allergy Clin Immunol 2017 Jul;140(1):242-248.e2. doi:10.1016/j.jaci.2016.09.051. Epub 2016 Nov 29
- Longhurst H (2018) Optimum Use of Acute Treatments for Hereditary Angioedema: Evidence-Based Expert Consensus. Front. Med. 4:245. doi: 10.3389/fmed.2017.00245








26 Comments
Excellent revision and a reminder to look outside the obvious!
Really interesting and useful module
Very informative session, well done.
EXCELLENT
GOOD article to understand HAE and differential diagnosis
Found this to be a very useful module. It’s one of those topics I learnt for undergrad exams and then didn’t think about much after, beyond the ACE-I angioedema of which I’ve seen a fair few cases. I particularly liked the WAO treatment breakdown, as I feel a bit more comfortable with the thought of having to see a HAE patient needing treatment.
Good article about HAE
nice one
EXCELLENT
very informative
Very useful informations with focus on the different types of medications and their uses
A good read to learn more about HAE
Very useful, thank you
Excellent module
Thanks, complicated immunology but good to have a bit more detail.
A clinically very important topic and an excellent module to read.
Very informative. Will definitely change my practice as a result.
Really good update & useful for revision purposes. Thankyou!
Excellent
I had no clue about the treatment modality until I came across this. Easy break down.
Thank you , informative topic
Very good
Interesting and a good read
I am working in the ED for so long, come across HAE often times, but never understood completely. very detailed presentation. very helpful. management is very informative and helpful. thanks very much.
Excellent and Very Informative
thanks