Author: Abel P Wakai / Editor: Jason Kendall / Reviewer: Stewart McMorran, Eugene Henry / Codes: CC4, CC9, CP2, ResP2, SLO1 / Published: 30/07/2021
Context and Definition
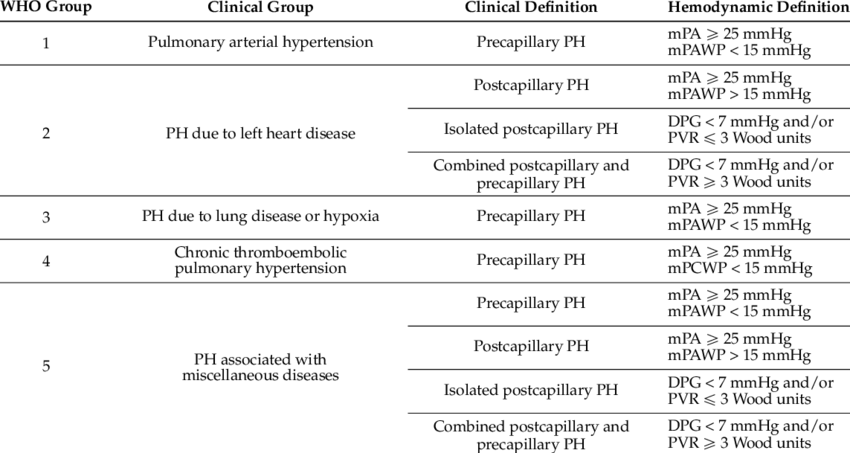
Pulmonary hypertension (PH) is an elevation in pulmonary vascular pressure that can be caused by an isolated increase in pulmonary arterial pressure or by increases in both pulmonary arterial and pulmonary venous pressures [1]. The World Health Organization (WHO) diagnostic classification of PH has 5 classes based on pathophysiology and aetiology.
Pulmonary arterial hypertension (PAH) is the most widely studied class of PH. It refers to conditions that share common isolated elevations in pulmonary arterial pressure, namely: sporadic PAH, familial PAH and PAH associated with other diseases (e.g. collagen vascular disease and congenital systemic-to-pulmonary shunts), PAH associated with drugs and toxins (e.g. appetite suppressants such as fenfluramine, cocaine and amphetamines).
PAH is haemodynamically defined as a resting mean pulmonary arterial pressure greater than 20 Hg with a normal pulmonary capillary or left atrial pressure (<15 mm Hg) [1-3]. The revised definition incorporates inclusion of pulmonary vascular resistance (PVR) ≥3 Wood units (WU) in the definition of all forms of pre-capillary PH.
PH is suggested when an echocardiogram-derived estimate of pulmonary arterial systolic pressure exceeds 40 mm Hg at rest.
Learning Bite
Pulmonary arterial hypertension is defined as a resting mean pulmonary arterial pressure greater than 25mmHg with a normal pulmonary capillary or left atrial pressure (<15mmHg).
Epidemiology
Pulmonary arterial hypertension (PAH) is a rare but probably underestimated condition.
No published data on the estimated prevalence of PH in developing countries is available. However, the prevalence of PH is thought to be much higher than reported in developing countries where diseases that may promote pulmonary vascular disease (schistosomiasis, sickle cell disease, human immunodeficiency virus infection, liver cirrhosis and congenital heart disease) are relatively common [4-6].
In Europe, the prevalence of PAH has been reported at 15-60 subjects per million population with an annual incidence of 5-10 cases per million per year.
PAH affects women more commonly than men, and patients of all ages may develop the disease. The mean age at diagnosis has been reported at 36 to 50 years, with more recent series and series including PAH related to other systemic diseases (particularly scleroderma) reporting older mean ages at diagnosis.[20]
The challenge
Although there is a paucity of data-driven evidence regarding acute problems in PH, patients with known PH may present to the emergency department (ED) with a variety of acute problems related to this disease:
- Pulmonary embolism
- Acute right heart failure
- Cardiac arrest
- Catheter-related sepsis
- Technical problems with intravenous catheters
- Pedal Edema
In addition, the emergency physician is in a strong position to consider the initial diagnosis in patients with previously undiagnosed pulmonary hypertension as long as there is a high index of suspicion in any patient presenting with breathlessness in the absence of an alternative cause of cardiorespiratory disease.
Pathophysiology
Several cellular mechanisms are implicated in the pathogenesis of PH [9]:
- Mutations in the bone morphogenetic protein receptor-2 (a member of the transforming growth factor-beta family)
- Allelic variations in the serotonin transporter (5-HTT)
- Reduced bioavailability of endogenous nitric oxide
- Alteration in the metabolism of cyclic nucleotides
- Imbalance in the metabolism of prostanoids (prostacyclin and thromboxane A2)
- Release of peptide mediators by the vascular endothelium (e.g. endothelin-1)
Prolonged PH can lead to right heart failure due to sustained increases in pulmonary artery pressure and right ventricle (RV) afterload.
Right ventricular function worsens in parallel to elevations of the pulmonary artery pressure. Chronic pressure overload stimulates the RV to hypertrophy over time. This hypertrophy, coupled with reduced contractility, causes a reduction in coronary blood flow to the RV myocardium, which can produce right ventricular ischaemia and dilation.
Right ventricular enlargement progresses to tricuspid annular dilation and regurgitation, and subsequent displacement of the inter-ventricular septum toward the left ventricle. Alterations in the left ventricle are then observed secondary to right ventricular overload. Left sided heart failure ensues, as evidenced by depressed left ventricular functional curves, and increased LV end diastolic and pulmonary capillary wedge pressures.
The cascade that follows is a slippery slope that leads to increased RV end diastolic pressure, lower extremity oedema, increased jugular venous pressures, congestive hepatomegaly, decreased oxygenation, decreased tissue perfusion, and ultimately, cardiovascular collapse.
Learning Bite
Patients with prolonged PH may present to the ED with acute right heart failure due to sustained increases in pulmonary artery pressure and right ventricle (RV) afterload.
Risk Stratification
The severity of PH can be clinically stratified according to World Health Organization (WHO) guidelines, a modification of the New York Heart Association (NYHA) functional classification(10,11) (see Box 3).
Functional Assessment in PH (WHO guidelines):
- Class I – Patients with pulmonary hypertension but without resulting limitation of physical activity. Ordinary physical activity does not cause undue dyspnoea or fatigue, chest pain or near syncope.
- Class II – Patients with pulmonary hypertension resulting in slight limitation of physical activity. They are comfortable at rest. Ordinary physical activity causes undue dyspnoea or fatigue, chest pain or near syncope.
- Class III – Patients with pulmonary hypertension resulting in marked limitation of physical activity. They are comfortable at rest. Less than ordinary activity causes undue dyspnoea or fatigue, chest pain or near syncope.
- Class IV – Patients with pulmonary hypertension with inability to carry out any physical activity without symptoms. These patients manifest signs of right heart failure. Dyspnoea and/or fatigue may even be present at rest. Discomfort is increased by any physical activity.
Learning Bite
Severe exercise limitation (World Health Organization [WHO] class IV), near syncope, syncope, or lower extremity oedema suggest advanced PH and require urgent referral to a specialist unit for evaluation.
History
The symptoms of PH are non-specific.
Progressive dyspnoea and fatigue that cannot otherwise be explained are the most common symptoms of PH. Although PH remains an uncommon cause of dyspnoea, a thorough evaluation of any patient presenting to the ED with dyspnoea in the absence of an alternative cause of cardiorespiratory disease is warranted.
What six pieces of information would you gather for a patient with a problem-focused history presenting with dyspnoea in the absence of an alternative cause of cardiorespiratory disease?
Answer:
- the type and level of activity associated with dyspnoea;
- timing of symptom onset and progression;
- associated symptoms, including chest pain, palpitations, lower extremity oedema, near syncope, syncope and fatigue;
- thorough review of cardiac, respiratory, rheumatological, neurological and haematological systems;
- family history of PH;
- drug history – particularly, use of aminorex, fenfluramine, SSRIs, amphetamines, cocaine, interferon alpha and beta, chemotherapeutic agents such as mitomycin C, cyclophosphamide
Physical examination
Findings on physical examination may suggest PH, or the presence of underlying conditions associated with PH.
List five physical signs that are suggestive of PH.
Answers:
Physical signs of PH include:
- Left parasternal heave
- Accentuated pulmonary component of the second heart sound
- Pansystolic murmur of tricuspid regurgitation
- Raised JVP
- Hepatomegaly
- Ascites
- Peripheral odoema
Other signs may suggest an underlying cause of PH such as:
- Telangiectasia and sclerodactyly in scleroderma;
- Inspiratory crackles in interstitial lung disease
- Spider naevia and palmar erythema in liver disease;
- Digital clubbing in cyanotic congenital heart disease, interstitial lung disease or liver disease
Learning Bite
PH should be considered in all patients presenting with dyspnoea in the absence of an alternative cause of cardiorespiratory disease.
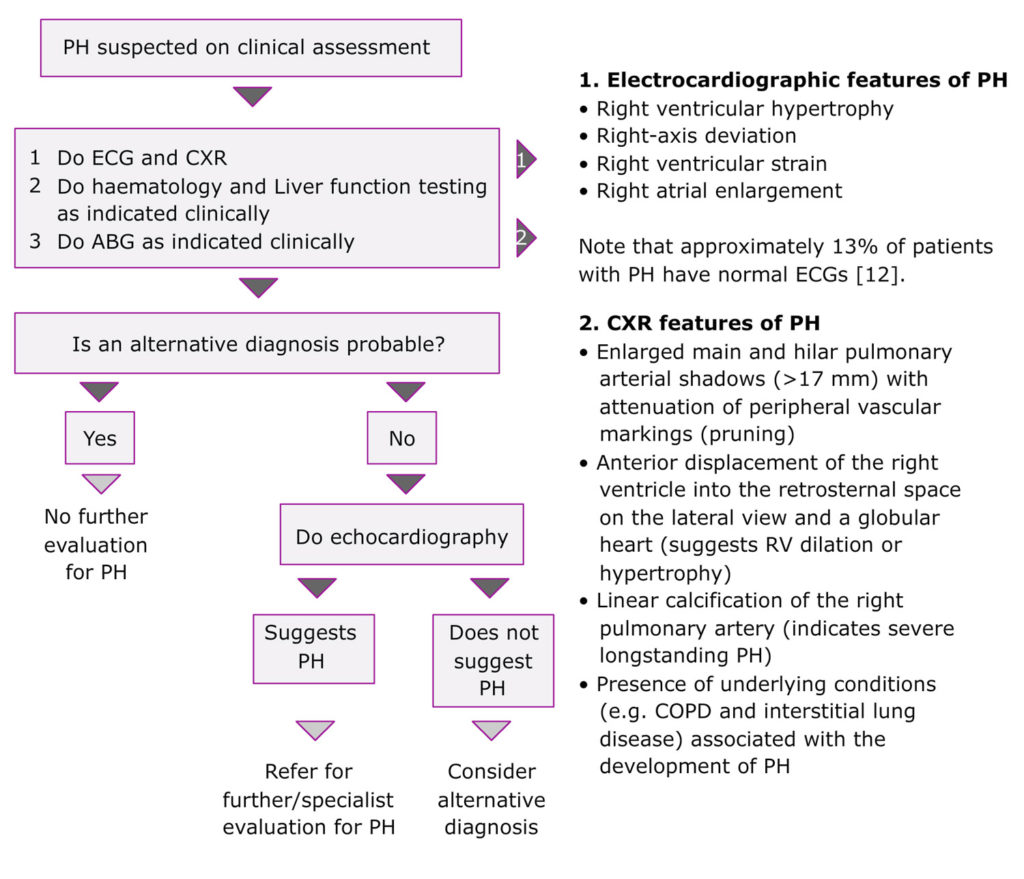
An ED-based diagnostic approach to a patient suspected of having pulmonary hypertension is required. In the ED, investigational tools for PH are generally limited to venous and arterial blood assays, electrocardiography and chest radiography. If PH is suggested after these initial investigations, the best screening investigation to confirm the diagnosis and determine referral to a specialist is echocardiography.
Learning Bite
While ECG and chest radiography are often abnormal at presentation, the sensitivity of these investigations is such that normal appearances do not exclude PH.
Doppler echocardiography is the best screening investigation for PH.
Management of the acutely ill patient with PH should include careful evaluation for secondary causes of decompensation (such as a low-grade line infection or pulmonary thromboembolism).
The management approach can be broadly divided into two stages: immediate ED management and subsequent or specialist management. Immediate ED management options are presented below.
| Problem | Intervension(s) required |
| Hypoxaemia | Supplemental oxygen |
| Arrhythmias |
|
| Volume overload |
|
| Acute right heart failure |
|
| Cardiac arrest | Advanced life support resuscitation while searching for underlying precipitant |
| Technical intravenous catheter and pump problems | Prompt restoration of intravenous therapy |
| Catheter-related infection |
|
| Bleeding in warfarinised PH patients |
|
Volume-overloaded Patients
For patients who are volume overloaded at presentation, diuresis—even against the background of marginal cardiac output and low blood pressure—may be required [27].
In a subset of patients, support with inotropes or pressors is necessary: animal data suggest a better haemodynamic response with sympathomimetic agents such as dobutamine, noradrenaline, and dopamine rather than vasopressin or phenylephrine; milrinone also has favourable effects on cardiac output but may lead to excessive hypotension [14-17].
Diuretics are indicated for right ventricular volume overload [1]. However, rapid and excessive diuresis may precipitate systemic hypotension and renal insufficiency [1]. Spironolactone, an aldosterone antagonist that is of benefit in patients with left-heart failure, is also used to treat right-heart failure [1]. Although not extensively studied in PAH, digitalis is sometimes used for refractory right ventricular failure [1,12]. In addition, atrial flutter or other atrial dysrthythmias often complicate late-stage right-heart dysfunction, and digoxin may be useful for rate control [1].
Subsequent specialist management
Because of the expertise required, specialist centres prefer to initiate administration of the drugs outlined in Box 8(1). Regarding subsequent (specialist) management, there has been recent interest in using a combination of drugs with different mechanisms of action for the management of PH. For example, phosphodiesterase inhibitors may enhance and prolonged the effects of prostanoids(1).
Similar to drug treatment of essential hypertension and cancer, combination drug therapy potentially enhances drug efficacy and may permit individual drugs to be used at lower doses, minimizing drug toxicity(1). Regarding the interventional and surgical therapies for PH, atrial septostomy is generally used as a palliative procedure or as a stabilizing bridge to lung transplantation when advanced medical therapy is not available (e.g. in developing countries)(19,20).
Subsequent (specialist) management:
- vasodilator testing and calcium-channel blockers
- prostanoids
- endothelin-receptor antagonists
- phosphodiesterase-5-inhibitors
- interventional and surgical therapies (eg atrial septostomy, lung transplantation)
Management Learning Bites
- Diuretics are indicated to reduce fluid retention in patients with PH
- Digoxin may be beneficial in heart failure due to PH, and should be considered in patients in sinus rhythm who remain symptomatic on medical therapy
- Establishing the diagnosis and aetiology requires early referral to a specialist PH unit
- If possible, all patients should be seen by a consultant in cardiology or respiratory medicine before referral to a designated centre
The main pitfall in the ED management of PH is not maintaining a high index of suspicion in the patient presenting with dyspnoea in the absence of an alternative cause of cardiorespiratory disease.
A patient with PH may present with symptoms that are very common in ED patients (e.g. dyspnoea, fatigue, chest pain, near syncope or syncope). The emergency physician should consider PH in the differential diagnosis for these symptoms. For example, a patient who presents to the ED with chest pain may be having an acute myocardial infarction for which sublingual glyceryl trinitrate (GTN) is appropriate; however if a patient with chest pain also has RV failure as a complication of PH, sublingual GTN may cause catastrophic hypotension and may be contraindicated.
A combination of investigations such as chest x-ray, ECG and point of care echocardiography may assist in differentiating between LV failure and RV failure at the bedside.
Grade of recommendation: D; Level of evidence: 5
- PH should be considered in all patients presenting with dyspnoea in the absence of an alternative cause of cardiorespiratory disease(21).
- While ECG and chest radiography are often abnormal at presentation, the sensitivity of these investigations is such that normal appearances do not exclude PH(21).
- Doppler echocardiography is the best screening investigation for PH(21).
- Diuretics are indicated to reduce fluid retention in patients with PH(21).
- Digoxin may be beneficial in heart failure due to PH, and should be considered in patients in sinus rhythm who remain symptomatic on medical therapy(21).
- Acute arrhythmias require prompt management with the aim of restoring sinus rhythm and preventing recurrence of the arrhythmia(21).
- Establishing the diagnosis and aetiology requires early referral to a specialist PH unit(21).
- If possible, all patients should be seen by a consultant in cardiology or respiratory medicine before referral to a designated centre(21).
- Sublingual glyceryl trinitrate may be contraindicated in patients with chest pain associated with decompensated right ventricular failure due to PH(21).
- Rubin LJ, Badesch DB. Evaluation and management of the patient with pulmonary arterial hypertension. Ann Intern Med. 2005 Aug 16;143(4):282-92.
- Rubin LJ; American College of Chest Physicians. Diagnosis and management of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004 Jul;126(1 Suppl):7S-10S.
- Rubin LJ. Primary pulmonary hypertension. N Engl J Med. 1997 Jan 9;336(2):111-7.
- Humbert M. Update in pulmonary arterial hypertension 2007. Am J Respir Crit Care Med. 2008 Mar 15;177(6):574-9.
- Humbert M, Khaltaev N, Bousquet J, Souza R. Pulmonary hypertension: from an orphan disease to a public health problem. Chest. 2007 Aug;132(2):365-7.
- Simonneau G, Galie N, Rubin LJ, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol 2004;43:5S-12S.
- Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med. 2006 May 1;173(9):1023-30.
- Peacock A, Murphy NF, McMurray JJV, et al. An epidemiological study of pulmonary arterial hypertension in Scotland. Eur Respir J 2007;30:104-109.
- Hoeper MM, Rubin LJ. Update in Pulmonary Hypertension 2005. Am J Respir Crit Care Med 2006;173:499-505.
- Rich S. Primary pulmonary hypertension: executive summary from the World Symposium on Primary Pulmonary Hypertension. Evian, France: World Health Organization; 1998.
- Edelman JD. Clinical presentation, differential diagnosis, and vasodilator testing of pulmonary hypertension. Semin Cardiothorac Vasc Anesth. 2007 Jun;11(2):110-8.
- Ahearn GS, Tapson VF, Rebeiz A, et al. Electrocardiography to define clinical status in primary pulmonary hypertension and pulmonary arterial hypertension secondary to collagen vascular disease. Chest 2002;122:524-527.
- Sandoval J, Aguirre JS, Pulido T, et al. Nocturnal oxygen therapy in patients with the Eisenmenger syndrome. Am J Respir Crit Care Med. 2001 Nov 1;164(9):1682-7.
- Acosta F, Sansano T, Palenciano CG, et al. Effects of dobutamine on right ventricular function and pulmonary circulation in pulmonary hypertension during liver transplantation. Transplant Proc 2005;37:3869-3870.
- Hirsch LJ, Rooney MW, Wat SS, et al. Norepinephrine and phenylephrine effects on right ventricular function in experimental canine pulmonary embolism. Chest. 1991 Sep;100(3):796-801.
- Leather HA, Segers P, Berends N, et al. Effects of vasopressin on right ventricular function in an experimental model of acute pulmonary hypertension. Crit Care Med 2002;30:2548-2552.
- Rich S, Gubin S, Hart K. The effects of phenylephrine on right ventricular performance in patients with pulmonary hypertension. Chest. 1990 Nov;98(5):1102-6.
- Rothman A, Sklansky MS, Lucas VW, et al. Atrial septostomy as a bridge to lung transplantation in patients with severe pulmonary hypertension. Am J Cardiol 1999;84:682-686.
- National Pulmonary Hypertension Centres of the UK and Ireland. Consensus statement on the management of pulmonary hypertension in clinical practice in the UK and Ireland. Thorax 2008;63 Suppl 2:ii1-ii41.
- 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The joint task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology and the European Respiratory Society. European Heart Journal, vol. 37, issue 1, 1 Jan 2016, pages 67-119.
- Simonneau G, Hoeper MM. The revised definition of pulmonary hypertension: exploring the impact on patient management. European Heart Journal Supplements. 2019; 21(Supplement_K):K4-K8.
- Connolly MJ, Kovacs G. Pulmonary hypertension: a guide for GPs. Br J Gen Pract. 2012;62(604):e795-e7.




2 Comments
Comprehensive module. PH is something we see frequently in patients with chronic lung disease but probably under recognise in other patients.
Excellent learning