Author: Max Sugarman / Editor: Nikki Abela / Codes: SLO1, SLO11, SLO12, SLO6, SLO8, SLO9 / Published: 29/10/2019
Medical student Max Sugarman tells RCEMLearning what triggered him to work on a hot debrief tool and how he went about implementing it.
During my time in the ED this year, I’ve come to appreciate that whilst the ED can be a place of unparalleled learning opportunities, it is also the setting for some of the most intimate and significant moments of the lives of patients and their families. Unfortunately, the outcomes of these situations can often be very difficult for those present to come to terms with.
Early in the year, myself and a student colleague were involved in our first cardiac arrest resuscitation attempt, which was sadly unsuccessful. I found it particularly difficult to process the grief of the family when experienced for the first time. As a medical student, I am aware that as my career progresses I will become more involved in these incidents and the development of effective coping mechanisms is vital. After the attempt, the team quickly dispersed. Despite my placement ED being an incredibly supportive environment, there was no debrief for the staff or students involved.
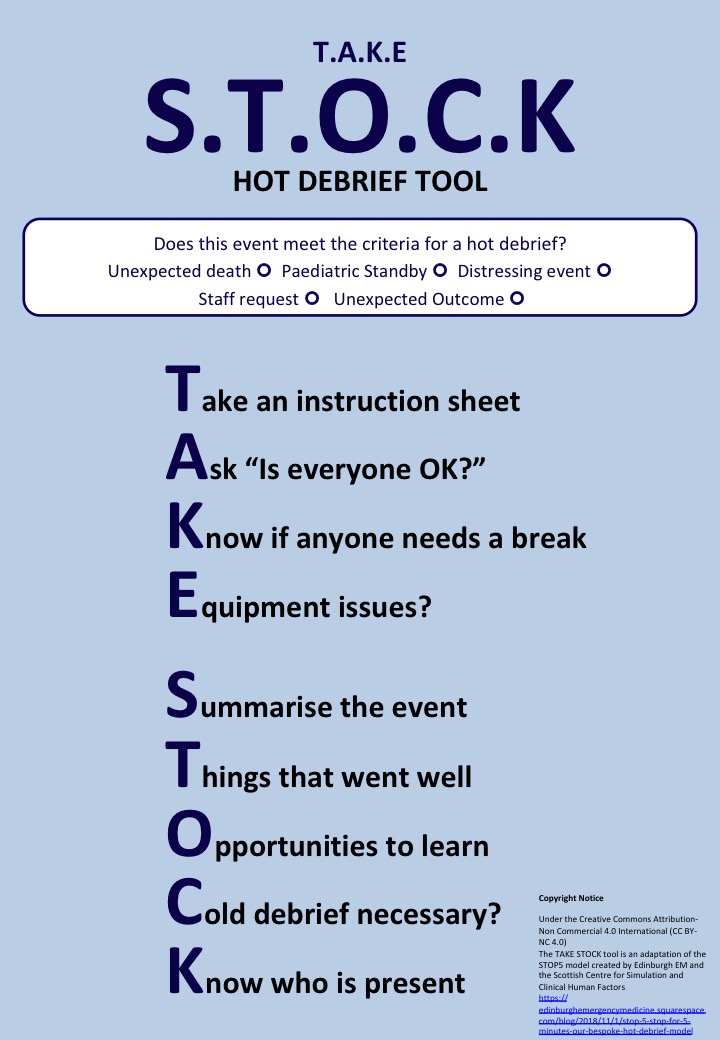
This experience led me to look into how these events, known as critical incidents, can impact the well-being of both students and staff. This formed the basis of my QI Project, and resulted in the development of the ‘TAKE STOCK’ hot debrief tool that is now being used in our department.
TAKE STOCK for 5 Minutes is an adaption of the STOP5 model created by Edinburgh EM and the Scottish Centre for Simulation and Clinical Human Factors
What is the impact of Critical Incidents on ED staff?
Critical Incidents (CIs) negatively affect the personal and professional capabilities of staff, the cumulative effects of which can potentially result in burnout. This places ED staff at exquisitely high risk.
As the recognition of human factors and staff wellbeing increases, the negative effects of burnout on patient care are beginning to be quantified. ED workload is increasing, and staff shortages due to stress-related illnesses are harming patients and staff, accounting for a significant proportion of abcesnces. Doctor empathy is reduced, and patient satisfaction suffers. Therefore, interventions to reduce burnout should be implemented and evaluated.
Debriefing is one such intervention. It occurs in two forms: cold debrief and hot debrief. Cold debriefing, a lengthy discussion occurring days after a CI, is the more common form.
Hot debriefing is a shorter process occurring immediately. It facilitates a ‘first response’ to the personal and professional needs of the team, allowing for open discussions around care, the opportunity for junior team members to ask questions, and also for any equipment errors to be immediately identified and actioned.
How can we make time to debrief?
Questionnaires distributed to staff in our ED indicated that time pressures was likely to be the biggest barrier to the performance of a hot debrief. Therefore, it was vital that a tool designed for immediate use wouldn’t take time away from the next patient, who is always waiting to be seen. If other emergency services can debrief as such a standard part of practice, what’s stopping Emergency Medicine from jumping on the bandwagon?
Therefore, through consultation with the staff within our department, we created the TAKE STOCK hot debrief tool adapted from the STOP5 model created by Edinburgh EM and the Scottish Centre for Simulation and Clinical Human Factors to meet the needs of the team in our ED.
How did the TAKE STOCK tool work in practice?
To promote the tool before introduction, we discussed it at both doctor and nursing handovers. Posters were placed around the department and in each resus bay. Once introduced, we encouraged debriefs to take place at every opportunity. Initially uptake was slow, but once it was realised that a hot debrief could fit into a busy environment, more and more were performed. The benefits of recording a list of names of those present ensured they could receive proper follow-up, and if a cold debrief was necessary then invites were sent out accordingly and without the challenges of looking back through case notes to find out who was there.
Taking it forward
Ultimately, debriefing from our experience has only been beneficial. It has been appreciated by team members of all levels of seniority and is currently being integrated into our trusts ‘death in theatre’ policy and introduced into a number of external trusts. One of the causes of the widespread lack of hot debriefing is the lack of a formal process. Both the STOP5 and TAKE STOCK tools provide this structure, resulting in an easy to follow process that won’t take time away from the other clinical demands in the department.
Thank you Sarah Langston, John Matthews, Pam Nelmes, Blair Graham and the rest of the team in Whiston ED for all your help with this QIP.
References
- Clark, R. and McLean, C. (2018) ‘The professional and personal debriefing needs of ward based nurses after involvement in a cardiac arrest: An explorative qualitative pilot study’, Intensive and Critical Care Nursing, 47, pp. 78-84.
- Couper, K. and Perkins, G. D. (2013) ‘Debriefing after resuscitation’, Current Opinion in Critical Care, 19(3), pp. 188-194.
- Dominguez-Gomez, E. and Rutledge, D. N. (2009) ‘Prevalence of secondary traumatic stress among emergency nurses’, Journal of Emergency Nursing, 35(3), pp. 199-204.
- Farley, H., Enguidanos, E. R., Coletti, C. M., Honigman, L., Mazzeo, A., Pinson, T. B., Reed, K. and Wiler, J. L. (2014) ‘Patient satisfaction surveys and quality of care: an information paper’, Annals of Emergency Medicine, 64(4), pp. 351-357.
- Fitzgerald, K., Yates, P., Benger, J. and Harris, A. (2017) ‘The psychological health and well-being of emergency medicine consultants in the UK’, Emergency Medicine Journal, 34(7), pp. 430-435.
- Healy, S. and Tyrrell, M. (2011) ‘Stress in emergency departments: experiences of nurses and doctors’, Emergency nurse , 19(4), pp. 31-37.
- Howard, L., Wibberley, C., Crowe, L. and Body, R. (2018) ‘How events in emergency medicine impact doctors’ psychological well-being’, Emergency Medicine Journal, 35(10), pp. 595-599.
- Maloney, C. (2012) ‘Critical incident stress debriefing and pediatric nurses: an approach to support the work environment and mitigate negative consequences’, Pediatric Nursing, 38(2), pp. 110-113.
- Mossburg, S. E. and Dennison Himmelfarb, C. (2018) ‘The Association Between Professional Burnout and Engagement With Patient Safety Culture and Outcomes: A Systematic Review’.
- Panagioti, M., Geraghty, K., Johnson, J., Zhou, A., Panagopoulou, E., Chew- Graham, C., Peters, D., Hodkinson, A., Riley, R. and Esmail, A. (2018) ‘Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis’, JAMA Internal Medicine, 178(10), pp. 1317-1330.
- Royal College of Emergency Medicine (2015) Medical and Practitioner Staffing in Emergency Departments.