Author: Lindsay Reid / Editor: Janet Skinner / Reviewer: Michael Perry, Grace McKay, Ahmad Alabood / Codes: GC1, GC2, GC6, GP7, SLO1 / Published: 15/06/2023
This session provides an overview of the assessment and management of patients presenting to the Emergency Department with jaundice.
Jaundice is not a disease but rather a clinical finding denoted by yellow discolouration of the skin, sclera and mucous membranes. Jaundice is caused by the deposition of bile pigment.
Patients may present to the Emergency Department with jaundice in isolation, or with other complaints and symptoms. Alone, jaundice has no adverse effects (except in the neonate).
It is the task of the Emergency Physician to evaluate the cause of jaundice by arranging appropriate initial investigations, and making a decision regarding the need for admission and further investigation and management.
In order to understand the physiology of jaundice, it is important to appreciate the normal physiology of haem metabolism.
Normal physiology
Normal haem metabolism can be divided into 3 stages, pre-hepatic, hepatic and post hepatic:
Pre-hepatic
As Red blood cells (RBC) reach the end of their lifespan (120 days) they pass through the reticulo-endothelial system in the spleen.
The RBCs are broken down by spleen macrophages into Haemoglobin, which is then further broken down into Haem and Globin.
The Globin portion is a protein which breaks down into amino acids.
The Haem portion is initially oxidised to form biliverdin, and then reduced to form Unconjugated Bilirubin. Unconjugated bilirubin travels to the liver, bound to serum albumin.
The majority of Bilirubin is produced from catabolism of haem with 425 and 510 mmol being made every day. 20% of Bilirubin comes from other haem sources, such as ineffective erythropoeisis, the break down of myoglobin in muscle and the breakdown of cytochromes and catalase.
Hepatic
In the liver an enzyme (UDP glucuronyl transferase) conjugates the bilirubin with glucuronic acid to form Conjugated Bilirubin.
Post-hepatic
Conjugated bilirubin is excreted in the bile into the small intestine. Enzymes within the small intestine covert conjugated bilirubin to stercobilinogen and urobilinogen.
Stercolbilinogen converts to Stercobilin and is excreted through faeces. Stercobilin is responsible for colouration of faeces.
Urobilinogen is filtered by the blood and transported to the kidneys where it is oxidised to form urobilin. Urobilin is excreted through urine and is responsible for the colour of urine.
Pathophysiology
The causes of jaundice can be divided into pre-hepatic, hepatic, and post hepatic aetiologies.
Pre-hepatic
Any process that causes an increased rate of RBC breakdown (haemolysis) and saturation of enzymes can cause jaundice.
- Malaria
- Sickle cell anaemia
- Spherocytosis
- Glucose-6-PD deficiency
- Haemolytic uraemic syndrome
- Transfusion reaction
Hepatic
Any process which effects liver function can cause jaundice.
- Drugs/toxins: Alcohol, paracetamol, anabolic steroids, Isoniazid, amanita toxin, chlorpromazine, flucloxacillin, halothane
- Infections: Viral hepatitis, infectious mononucleosis, leptospirosis
- Metabolic: Wilsons disease, Reyes disease, haemochromatosis
- Granulomatous: Wegners granulomatosis, lymphoma, Sarcoidosis, mycobacterial
- Genetic: Gilberts syndrome, Crigler-Najjar syndrome, Dubin-Johnson Syndrome
- Other: Fatty liver of pregnancy, primary biliary cirrhosis, amyloidosis, metastatic carcinoma, neonatal jaundice
Post-hepatic
Any process which causes post-hepatic obstruction can cause jaundice.
- Drugs amitriptyline, prochlorperazine, verapamil, co-amoxiclav
- Gallstones
- Pancreatic carcinoma
- Primary sclerosing cholangitis
- Biliary atresia
- Bile duct strictures
- Cholangiocarcinoma
- Pancreatitis
- Pancreatic pseudocyst
An accurate history and examination will help to identify factors that differentiate the causes of jaundice.
History
It is important to ask about the following risk factors:
- Alcohol intake
- Transfusion of blood products
- Sexual contact with a person known to have hepatitis or promiscuous sexual activity
- Intravenous drug misuse
- Recent tattoos or body piercings
- Recent foreign travel
- Needle stick injury
Clinicians should also specifically ask about
- Colour of urine and stool
- Weight loss
- Family history of jaundice
Learning Bite
Eliciting an accurate history is vital when looking for the cause of jaundice
Examination
A full examination may provide clues as to the cause of jaundice.
A hard nodular liver on a background of known malignancy may indicate metastatic disease.
Signs such as palmar erythema, spider naevi, proximal muscle wasting/weakness, hepatic flap, fetor hepaticus, cerebellar signs or encephalopathy may indicate alcoholic liver disease.
Fever and right upper quadrant tenderness in association with jaundice are known as Charcots Triad, characteristic of acute cholangitis.
Painless jaundice and cachexia and an epigastric mass suggests biliary obstruction due to malignancy
Jaundice will be apparent when the serum bilirubin is 3x above normal. (The normal value of bilirubin is
Urinalysis
Pre-hepatic hyperbilirubinaemia Unconjugated bilirubin is bound to Albumin and is not water-soluble therefore cannot appear in the urine.
Post-hepatic hyperbilirubinaemia Conjugated bilirubin is water-soluble and therefore appears in the urine. Urobilinogen is absent due the inability of conjugated bilirubin to be excreted in to the small intestine.
The findings in the urine should then be confirmed by measuring direct (conjugated) and total bilirubin levels
Liver Function Tests
Liver function tests (LFTs) are the central test when investigating jaundice and often point towards the cause.
Other blood tests include:
- Full blood count: Raised reticulocyte count, Schistocytes on blood film and positive Coombs test indicates haemolysis.
- Amylase: If raised may indicate pancreatitis
- Hepatitis serology (for viral hepatitis)
- Autoimmune markers: such as Anti-nuclear antibodies and anti-smooth muscle antibodies, the presence indicates auto-immune disease. The majority of patients with PBC have anti-mitochondrial antibody. Up to 85% of patients with PSC have anti-nuclear cytoplasmic antibody
- Alpha 1 Antitrypsin: Deficiency may precede liver cirrhosis.
- Copper/Ceruloplasmin: Deficiency may indicate Wilsons Disease.
- Ferritin: Levels >1000ng/ml and transferrin saturations > 50% will indicate Haemochromatosis.
Imaging
The majority of diagnostic imaging in patients with jaundice will be performed external to the emergency department.
Abdominal UltraSound Scan (USS)
Abdominal USS is a useful initial radiological test to distinguish between hepatocellular and extra-hepatic causes. It is cheap, readily available, lacks radiation and is more sensitive than CT at detecting stones in the gallbladder. The drawback of USS is that it is limited at detecting intraparenchymal disease of the liver or pancreas, and it is operator-dependent.
Computed Tomography (CT)
CT is good at determining intraparenchymal liver and pancreas disease. Neither USS or CT are good at delineating intraductal gallstones.
Magnetic Resonance Cholangio-Pancreatography (MRCP)
MRCP is a non invasive, radiation free diagnostic test. It is useful for evaluating the biliary tree, pancreas and liver. The findings of the MRCP will determine whether a more invasive ‘ERCP’ is required.
Endoscopic Retrograde Cholangio-Pancreatography (ERCP)
ERCP may be required to detect disease in the biliary and pancreatic ducts which may be missed on CT and USS. As well as a diagnostic adjunct, it may be used therapeutically to remove gallstones from the biliary tract or to place stents across narrow ducts. The most common and serious complication of ERCP is pancreatitis.
Liver biopsy
Liver biopsy is used when serum and radiological investigations fail to provide a definitive diagnosis. Liver biopsy is particularly useful in diagnosing autoimmune hepatitis or biliary tract disorders (such as PBC or PSC)
Learning Bite
Abdominal USS is the most useful first-line imaging investigation in a patient presenting with jaundice
Often the course of jaundice will be indolent and therefore the emergency physician may only be involved in facilitating the initial investigations and management with a decision as to whether the patient should be admitted or discharged. However, it is important to remember that jaundice can reflect a medical emergency. These cases include:
- Ascending cholangitis
- Fulminant hepatic failure
- Massive haemolysis
- Neonatal jaundice
Timely diagnosis, resuscitation and initiation of therapy in these situations should occur. Patients with jaundice and anaemia due to haemolysis require admission.
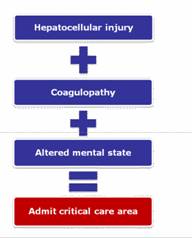
Patients with raised Alkaline Phosphatase and GGT are likely to have biliary tract obstruction and should have an USS requested in the ED and appropriate surgical/GI referral depending on the findings. Patients with raised AST/ALT have hepatocellular injury and should be admitted if there is evidence of:
- Coagulopathy
- Sepsis
- Altered mental status,
- Intractable pain/vomiting
- Otherwise outpatient investigation may be appropriate.
Acute Liver Failure
Patients with hepatocellular injury, coagulopathy, and altered mental status may have acute liver failure also known as ‘Fulminant Hepatic Failure’ (FHF).
Patients presenting with FHF require fluid resuscitation, haemodynamic monitoring, and admission to a critical care area for supportive care.
The most common causes of FHF are Paracetamol poisoning (in the UK) and acute Hepatitis B (worldwide).
Prior to liver transplantation, the mortality of FHF was greater than 80%.
Paracetamol Poisoning
The management of Paracetamol poisoning depends upon the quantity of Paracetamol ingested and the time since ingestion.
Always refer to ToxBase when managing poisoned patients.
Within 1 hour of overdose
Activated charcoal can be given as decontamination (absorption from the gut is usually complete within two hours).
If the quantity is potentially life threatening, gastric lavage is thought to be useful. Contraindications to lavage are patients who have a compromised, unprotected airway.
Within 8 hours of overdose
N-Acetyl Cysteine is proven to reduce the risk of serious hepatotoxicity.
Indications for consideration of liver transplant:
- Acidaemia (pH <7.3)
- Renal insufficiency
- Hepatic encephalopathy
- Elevated PT
pH < 7.3
or
In a 24h period, all 3 of:
- INR > 6 (PT > 100s) +
- Cr > 300mmol/L +
- grade III or IV encephalopathy
Pregnancy and neonatal jaundice
Any pregnant jaundiced patient should be managed in conjunction with the obstetrician. Patients who present with jaundice in the third trimester may require delivery.
Well appearing neonates with a bilirubin <15mg/dL can safely be discharged home with close outpatient follow-up. Neonatal jaundice can often be physiological due to increased break down of premature erythrocytes and insufficient Glucuronyl Transferase in the newborn liver but jaundice persisting after 2 weeks requires investigation. Neonatal jaundice is treated with phototherapy. Quick and accurate treatment of neonatal jaundice reduces the risk of development of kernicterus, deposition of bilirubin in the basal ganglia. Exchange transfusion is an aggressive treatment to lower bilirubin levels.
- Understanding Haem metabolism is key to understanding jaundice.
- The differential diagnosis of jaundice is very wide.
- LFTs are the key Emergency department investigation in jaundice. (grade 4, recommendation D)
- Abdominal USS is useful and readily available as first line imaging in the ED. (grade 3, recommendation D)
- Patients with coagulopathy, sepsis or altered mental status must be admitted. (grade 4, recommendation D)
- Ascending cholangitis, fulminant hepatic failure, massive haemolysis and neonatal jaundice reflect medical emergencies (grade 4, recommendation D)
- Assuming if USS is negative that there is no intraparenchymal disease of liver or pancreas.
- False negatives for bilirubin in the urine occur with Rifampicin.
- False positives for urinary urobilinogen occur in acute porphyria.
- Hypervitaminosis A or high levels of carotene can cause a paitent to appear jaundice but will have normal bilirubin levels
- National Institute for Health and Care Excellence. Jaundice in adults. NICE CKS, Last revised 2020.
- BMJ Best Practice – Assessment of Jaundice. London: BMJ Publishing Group, 2019. Last updated: 07 Feb 2023
- Cadogan M. Bilirubin and Jaundice. Life in the Fast Lane, 2023.
- Nickson C. Liver Transplantation for Paracetamol Toxicity. Life in the Fast Lane, 2020.








6 Comments
good striaght to the point overview of jaundice. thanks
Great refresher
brilliant article
Very good article
A very good introduction to pre, hepatic and post hepatic causes. And interpretatation of LFTs and the use of USS Abdo.
FOcused reference for a swift review of the approach to jaundice in ED