Authors: Jonathan Matthews, Rajan Atwal / Editors: Paramjeet Deol, Shashank Patil, Jorge Leon-Villapalos, Chris Gray, Lauren Taylor / Reviewer: Chris Gray / Codes: SLO4, SLO5, TP1, TP8 / Published: 11/02/2021
- Burns are a major public health problem globally. In addition to physical damage, they can leave a long lasting psychological and social impact.1,2
- In the UK 130,000 people each year visit the Emergency Department with burn injuries.2
- Approximately 8% (10,000) of these patients are admitted.2
- Although the majority of burns injuries in the UK are not life threatening, there are still around 200 deaths a year.3
A burn is defined as a traumatic injury to the skin or other organic tissue primarily caused by thermal or other acute exposures.
There are various types of burns which include:
- Thermal: This is the most common type of burn and includes flame burns, scalds (from hot liquids) and contact burns (from hot objects e.g. an iron or radiator).
- Chemical: Acids and alkalis found in household chemical products can produce very deep burns through coagulative and liquefactive necrosis.4 They will continue to burn the skin until completely removed. It is therefore essential that the skin is thoroughly irrigated.4 Alkalis penetrate deeper than acids and those presenting with alkali burns (commonly due to cement) will require immediate attention.
- Electrical: As an electrical current travels through the body it creates an entry and exit point, damaging tissue along its path as it is converted from electrical to thermal energy. Electrical burns from domestic low voltage exposures tend to be less severe than high voltage electrical burns which can cause extensive tissue damage and limb loss. It is still very important that domestic electrical burns are taken seriously and an ECG is performed as the alternating nature of domestic current can cause arrhythmias.
- Cold exposure (frostbite): These burns are caused by ice crystals which can form both intra and extracellularly.5 The subsequent fluid and electrical fluxes cause cell membrane lysis and cell death and a damaging inflammatory process is set up.5
- Radiation: Radio frequency energy or ionising radiation causes tissue damage. The most common type of radiation burn is sun burn.5 Other patients at risk of getting radiation burns are those undergoing radiation therapy for cancer treatment.
- Overall, flame injuries are the most common cause of burns, followed by scalds. Electrical and chemical injuries are much less common.1
- However, the types of burn sustained are different in different groups of people; in children the most common type of burn is a scald, whereas in adults flame burns are the most common.1,6
- Figure 1 shows the causes of burns by type and figure 2 shows the incidence of burns by age.


High risk groups in burns:
- Children: infants and toddlers up to 4 years old make up 20% of all patients with burn injuries.6 Seventy percent of their injuries are scalds due to spilling hot liquids or being exposed to hot bath water.6
- Older adults: People over the age of 65 make up around 10% of patients with burns. This may be due to slower reactions, mental and physical co-morbidities and immobility.1, 6 This group tends to have a higher incidence of burns during the winter months.
- Other higher risk groups include: alcoholics, epileptics, those with chronic psychiatric or medical conditions and those who have a low socio-economic status.1,6
Learning bite
In children and vulnerable adults, it is important to actively exclude non-accidental injury.
Burn injuries result in both local and systemic responses
Pathophysiology Local response
Jacksons Burn wound model is made up of 3 zones (figure 3). This helps us to understand the pathophysiology of a burn injury.
- Zone of Coagulation: occurs at the point of maximum damage i.e. the nearest point to the heat source. There is irreversible tissue necrosis here due to coagulation of proteins.
- Zone of Stasis:surrounding the zone of coagulation, this area is characterised by decreased tissue perfusion. It is damaged but potentially viable. If the burn is managed correctly it has the potential to be salvaged, otherwise it could evolve into an area of necrosis.
- Zone of Hyperaemia: the outermost zone as its name suggests is where there is increased tissue perfusion. This is a reversible zone.
- The release of cytokines and other inflammatory mediators at the site of injury has a systemic effect once the burn reaches 20- 30% of total body surface area.
- Cardiovascular changes Capillary permeability is increased, leading to loss of intravascular proteins and fluid into the interstitial compartment. Peripheral and splanchnic vasoconstriction occurs. Myocardial contractility is decreased. These changes, coupled with fluid loss from the burn wound, result in systemic hypotension and end-organ hypoperfusion.
- Respiratory changesInflammatory mediators cause bronchoconstriction, and in severe burns, adult respiratory distress syndrome can occur.
- Metabolic changesThe basal metabolic rate increases up to three times its original rate. This, coupled with splanchnic hypoperfusion, necessitates early and aggressive enteral feeding to decrease catabolism and maintain gut integrity.
- Immunological changesNon-specific down regulation of the immune response occurs, affecting both cell mediated and humoral pathways.

As with any major trauma, a systematic ABCDE approach to the primary survey is critical to ensure that any life threatening issues are not missed9,10. This will be outlined over the next few pages.
Assessment, investigation and management occur simultaneously at each stage of the approach. 9,10,11
Airway
The airway is at risk by three major mechanisms:
- Generalised oedema as a systemic response from an increasing burn size and depth can cause swelling of the airway and compromise airflow9, 10.
- Localised oedema as a result or direct thermal damage to the airway can obstruct airflow9
- Inhalation injury as a result of heat, smoke or toxic chemicals can cause damage to the airway.9
Assessment
Factors that increase the suspicion of airway obstruction or inhalation injury include: 10
| Hoarse voice |
| Respiratory distress/ stridor |
| Carbonaceous sputum |
| Singed nasal/facial hairs |
| Inflamed oropharynx |
| Burns to the face/oropharynx |
| History of burns in an enclosed space |
| Raised blood gas carbon monoxide (CO) level |

adapted from Airway swelling after laryngeal burn induced by swallowing hot food: Korean J Otorhinolaryngol-Head Neck Surg. 2015 Sep;58(9):634-636.
https://synapse.koreamed.org/ViewImage.php?Type=F&aid=507327&id=F1&afn=38_KJORL-HN_58_9_634&fn=kjorl-hns-58-634-g001_0038KJORL-HN
Management
- Sit patient upright9
- Any suspected airway injury necessitates senior anaesthetic review to identify and predict deterioration9.
- If indicated, early intubation with an uncut tube9 prevents the tube moving in the event of further swelling10
Common pitfall:
Failure to recognise or predict the deteriorating airway.
Gas exchange can be compromised for a number of reasons:
- Direct damage from inhalation injury to lower airways and gas exchange surfaces
- Carbon monoxide (CO) can quickly build up impairing oxygen carrying capacity 9,10.
- Burnt tissues with significant loss of the elasticity in superficial fibres are known as an eschar. This creates a constricting effect and inhibits expansion (figure 11). When circumferential around the chest/torso/neck this can lead to impaired chest expansion and subsequent ventilation issues9,10,11

Assessment:
- Exposure of the chest to assess for any injuries, and adequacy of ventilation
- Prompt assessment of oxygenation with a saturation probe9,10,11
- Baseline blood gas (to assess oxygenation, ventilation, and carbon monoxide9,10,11
Management
- Initially high flow oxygen (bear in mind that peripheral saturation readings may be falsely elevated with raised carbon monoxide levels), which can be later titrated to target appropriate saturations9,10
- Immediate discussion with burns centre if any restriction of movement of chest9,10
- Suspected inhalation injury may warrant intubation9,10
Common pitfalls:
- Failure to recognise rising CO level
- Failure to recognise poor ventilation and the need for escharotomy
Top tips:
- Escharotomy can be a lifesaving procedure that relieves restriction of movement and allows chest expansion. This is an emergency situation this will be discussed later
- Cyanide poisoning is common in patients that have been exposed to inhalation of burnt household items. In profound hypoxia consider early administration of cyanokit .10
- Burns >15% total body surface area (TBSA) in Adults and >10% in children can cause profound circulatory shock that can occur from both large fluid losses through tissue damage and from a systemic inflammatory response10.
- Haemodynamic instability is rarely due to the burn alone and should prompt us to look for other causes
- Circumferential limb burns can compromise blood supply distally
Assessment
- A thorough assessment of the extent of a burn is paramount: Burns <15% in adults and <10% in children do not require immediate fluid resusitation9
- Capillary refill time (CRT), blood pressure and mucous membrane assessment are important indicators of hydration status but may be hard to measure due to location of the burn10.
- Though rarely immediately helpful in the Emergency Department setting, early catheterisation is important as urine output is a reliable sign that can demonstrate poor perfusion and serve as a guide to ongoing resuscitation9, 10, 13.
- In a significant burn there can be an increased metabolic demand on the patient which can cause organ dysfunction. Therefore, important baseline tests to consider are full blood count, urea and electrolytes, coagulation profile, liver function tests, amylase, C-reactive protein and capillary blood glucose. This also helps to identify any other issues impacting on the patient. If the patient is likely to go to theatre a serum group and save is warranted.
- In circumferential limb burns, blood supply to the extremities should be checked regularly. If unable to do this clinically, a Doppler ultrasound can be used9,10, 11, 13.
Management
- Immediate intravenous (IV) access and, if required, fluid resuscitation are critical steps in initial care9, 10, 11, 13.
- Blood tests
- Evaluate any areas of circumferential burns in limbs and constantly reassess perfusion
- Any deterioration in the circulation to a limb could indicate ischaemia or a compartment syndrome. This warrants immediate discussion with a burns centre and may require urgent intervention such as escharotomy or fasciotomy9,10.
Top Tips
- IV access is paramount. If it is not possible to get IV or IO access through unburnt skin, access is mandated through burnt tissue.
- Creatine kinase is a useful test to perform to assess muscle breakdown9.
Like any trauma patient disability and exposure cannot be ignored.
Appropriate exposure is fundamental for the assessment of patients with burns. A thorough assessment of size and depth of burns is impossible without full exposure and a good secondary survey9,10,11,13. However patients with burns are physiologically vulnerable to getting cold so it is critical to keep them warm and minimise fluid loss9,10.
Management
- Consideration should be made to maintain body temperature by both active and passive warming.9, 10 This is balanced with the need to adequately expose the burn in order to assess, photograph and clean.10.
- Clean the burn with normal saline and cover with strips of cling film. Do not use cling film on the face.
- Consider imaging e.g. X-ray, CT etc. based on findings of the secondary survey
Common pitfalls
- Missing other injuries not related to burns g. traumatic head injury or long bone fractures in a blast injury
- Failure to give adequate analgesia
Top tip
- Have all members of the team present during exposure of an area to simultaneously evaluate and photograph the areas to avoid repeated unnecessary exposure and heat loss
The burning process is exceptionally painful and analgesia should be given early. Both pharmacological and non-pharmacological methods should be used to control pain.
- Non-pharmacological methods include cooling the burn under cold running water and covering with cling film. Cling film also helps to reduce heat loss and the risk of infection.
- Pharmacological treatment includes simple analgesia such as paracetamol and NSAIDs, as well as stronger analgesia like opioids and ketamine.
To guide management goals, it is important to assess both extent and depth of the burn.
To assess the extent of a burn it is vital to expose all areas of the body to accurately estimate percentage TBSA affected. This is essential to:
- Decide whether the patient requires fluid resuscitation (>10% TBSA in children or >15% TBSA in adults)
- Calculate the fluid requirement during the initial resuscitation period if needed
Common ways to estimate %TBSA are
- Lund and Browder charts (fig 12a)
- Using the patient’s palm (including finger and thumb surfaces) as an estimate of 1% TBSA
- Rule of 9s (fig 12b)
- Mersey Burns App (fig 12c) which enables the user to highlight areas of burn tissue on a model to accurately estimate %TBSA affected

adapted from: https://rphcm.allette.com.au/publication/cpm/Burns.html

Ref: Modified from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC449823/
**Link to app store Mersey burns app store**
Not all of the burn area would necessarily be included in the %TBSA calculation. The depth of burn needs to be considered.
Top tip
- Epidermal burns are not included when calculating the burn %TBSA
To make an accurate assessment of the depth of a burn, skin needs to be cleaned, blisters removed (except for small non-tense blisters [<6mm]) and capillary refill time tested.
Guidance on which blisters to de-roof and how to do it by the London and South East of England Burn Network (LSEBN) can be found here.
- http://www.lsebn.nhs.uk/website/X13911/files/LSEBN%20Burns%20Blister%20Management.pdf
- http://www.lsebn.nhs.uk/website/X13911/files/LSEBN%20Burn%20Blister%20Deroofing%20Guideline.pdf
The depth of the burn can be classified into 1 of 4 types. The British Burn Association (BBA) accepted definition has replaced the older 1st, 2nd and 3rd degree classification.
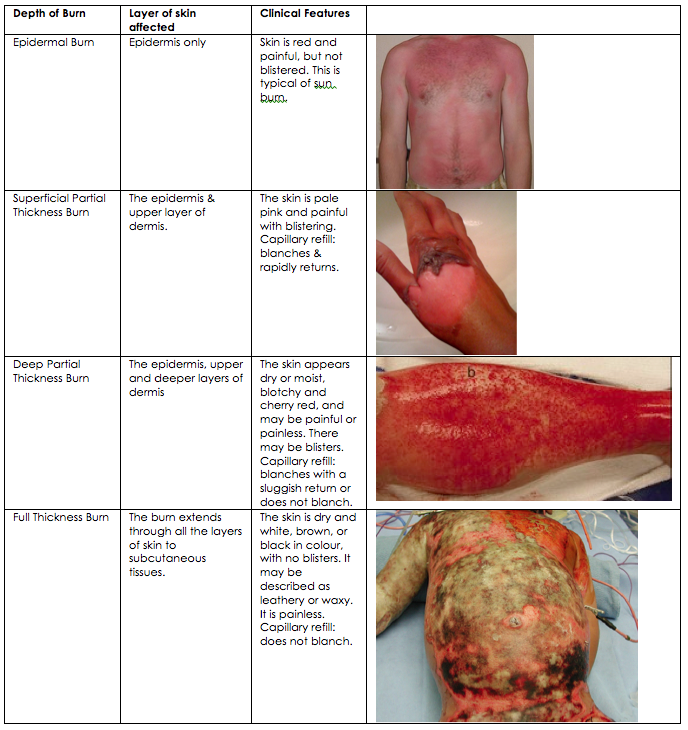
[Table adapted from reference 7 & 8]
- In clinical practice burn wounds are not homogenous but often are of mixed depths, as shown in Figure 15
 Figure 15
Figure 15
Property of Burns unit, Chelsea & Westminster Hospital
The white areas are Full Thickness burns (FT), with the deeper red and paler pink areas showing Deep Partial Thickness (DPT) and Superficial Partial thickness (SPT) burns respectively.
Depth of burn – Summary
In summary, assessing the depth of a burn is necessary to determine what the patient needs immediately, and what they may require going forwards in their management.
The distinction between epidermal burns (erythema) and those that are deeper is necessary as epidermal burns are excluded from the %TBSA calculation when deciding on the need for resuscitation and fluid management.
The distinction between full thickness burns and anything more superficial is necessary as those with full thickness burns, depending on location, are at risk of ventilatory problems or limb ischaemia and may require urgent surgical intervention.
Learning bite
The distinction between different types of partial thickness burns is not clinically relevant to the emergency practitioner. Only the inclusion of full thickness, and exclusion of epidermal burns aids in management.
Adults with burns >15% TBSA and children with burns >10% TBSA require fluid resuscitation. There are a number of methods to calculate appropriate fluid requirements. The most frequently used is the Parkland formula21:
2-4ml x weight in kg x %TBSA
- This estimates the total resuscitation fluid required over 24 hours from the time of the burn
- This is in addition to the usual maintenance fluid requirement
- Usually 3ml is used for the calculation
- 2ml might be considered in children or those at risk of complication from fluid overload
- 4ml might be considered in inhalational injuries where fluid losses are likely to be greater
- Half of the calculated volume should be administered within the first 8 hours from the time of the burn
- The remaining half should be administered over the subsequent 16 hours
- The optimal fluid choice is warmed balanced crystalloid, such as Hartmann’s Solution or Plasmalyte
- Urine output should be monitored closely and input titrate to achieve an output of >0.5mg/kg/hr in adults and >1ml/kg/hr in children <30kg
- Urine output targets should be doubled if rhabdomyolysis is suspected
1. REMOVE
Remove loose clothing and all jewellery. Do not remove anything that is adherent or melted
2. COOL
Irrigate and cool thermal burns with cool (15°C) running tap water for 20 minutes. This can be beneficial up to three hours post-burn injury and should be done in the emergency department if not carried out in full prehospitally
Irrigate chemicals from skin/eyes immediately with warm running water for at least 15 minutes (though irrigation periods longer than this are usually required)
Do not use ice/iced water/ice packs/gel based cooling products for this purpose
3. COVER
Clean the wound with normal saline and cover any areas of skin loss with cling film
Do not use cling film on the face
Do not wrap cling film circumferentially around a limb (this creates a constrictive eschar)
Cover chemical burns with a non-adherent dressing
Tetanus status should be considered though latest guidelines would only consider a burn to be tetanus-prone in conjunction with signs of systemic sepsis9,10,22
Management of the burn wound – electrical
The initial management of patients presenting with electrical burns is unchanged from that already described, however there are key differences to bear in mind.
In contrast to thermal burns, deeper tissue damage may be far more extensive than any superficial wounds may suggest and may involve whole compartments of the limbs. In patients with electrical burns to a limb, a high level of suspicion of compartment syndrome should be maintained.
Tissue damage from electrical burns may also lead to renal failure due to the release of haemochromogens into the circulation. For this reason, if the urine is pigmented, urine output targets should be doubled (to 1ml/kg/hr in adults or 2ml/kg/hr in children).
An ECG should be obtained on admission for every patient presenting with an electrical burn. However, if the patient is asymptomatic and the ECG is normal, then there is no need for further cardiac monitoring or admission.23
In certain circumstances, patients should be referred to specialist burn services.
The minimum threshold for referral suggested by the British Burn Association can be summarised as:
- All burns ≥2% TBSA in children or ≥3% TBSA in adults
- All full thickness burns
- All circumferential burns
- Any burn not healed in 2 weeks
- Any burn with suspicion of non-accidental injury should be referred to a burn unit/centre for expert assessment within 24 hours
In addition, the following factors should prompt a discussion with a consultant in a specialised burn care service and consideration given to referral:
- All burns to hands, feet, face, perineum, or genitalia
- Any chemical, electrical or friction burn
- Any cold injury
- Any unwell/febrile child with a burn
- Any concerns regarding burn injuries and co-morbidities that may affect treatment or healing of the burn
If the above criterie not met, continue with local care and dressings as required
If the burn wound changes in appearance or there are signs of infection or concerns regarding healing, then discuss with a specialised burn service
If there is any suspicion of toxic shock syndrome (TSS) then refer early. Consider this in any patient with any size burn, presenting with:
- Pyrexia
- Rash
- Diarrhoea/vomiting
- General malaise
- Anorexia
- Tachycardia/tachypnoea/hypotension
- Reduced urine output
Local referral policy may differ and should be followed. Local centres may also have an online referral method with the capability to send photographs of burns in a secure way, which can be extremely useful.
With full thickness and deep partial thickness burns, the dermis can become very stiff. If this occurs circumferentially over the chest it can restrict chest wall movement and lead to mechanical respiratory failure. Equally if there are circumferential burns to the limbs this can cause limb ischaemia. In these cases an emergency escharotomy needs to be undertaken to release the rigid skin to allow: adequate ventilation (if the chest is involved) or circulation (in the limb).19
The process of the dermis stiffening takes time and the majority of patients requiring escharotomies often go to theatre for this at a later stage. However, knowledge of the procedure can be life and limb saving in the emergency setting.
Procedure:
- The limb should be kept in the anatomical position.
- The area is cleaned and incised along the anatomical lines (see figure 11) with a scalpel down to the fat
- The incision should not go down to the muscle or fascia
- For the limbs the incisions need to release both medial and lateral aspects
- For the chest the incision needs to release the whole breast plate

- Peck MD: Epidemiology of burn injuries globally, uptodate.com, Topic 822 Version 13.0, 2016
- NHS commissioning board: Specialised Burn Care (All Ages), Service specification D06/S/a, 2013
- Benson A, Dickson WA, Boyce DE: Burns, BMJ 649-652, 2006
- Hettiaratchy S, Dziewulski P: Pathophysiology and types of burns, BMJ 1427-1429, 2004
- Rice PL, Orgill DP: classification of burns, uptodate.com, Topic 819 Version 12.0, 2016
- Hettiaratchy S, Dziewulski P: ABC of burns introduction, BMJ 328:1366, 2004
- British Burn Association: European practice guidelines for Burn Care Based by the Copenhagen EBA meeting, September 2002
- The depth of the burn can be classified into 1 of 4 types. The British Burn Association (BBA) accepted definition has replaced the older 1st, 2nd and 3rd degree classification.
- Clinical Knowledge Summaries: Burns and scalds, 2015
- American College of Surgeons ATLS Course Manual 9th Ed Chapter Thermal Injuries, 2012
- London and South East Burns Network Initial Management of Severe Burns, 2015
- Stander et al The emergency management and treatment of Severe burns Emergency medicine International 2011; 2011: 161375.
- Remote PHC Manuals Burns, 2014
- Hettiarachy et al Initial management of burns II assessment and resuscitation BMJ 2004 Jul 10; 329(7457): 101103.
- Mersey Burns St Helens and Knowsley teaching hospital NHS trust, 2014
- Barnes et al The Mersey Burns App: evolving a model of validation EMJ Emerg Med J doi:10.1136/emermed-2013-203416
- Hoon et al Airway Obstruction after Laryngeal Burn Induced by Swallowing Hot Food Korean J Otorhinolaryngol-Head Neck Surg. 2015 Sep;58(9):634-636. Korean.
- Gillies et al Use of cut endotracheal tubes should be avoided in the initial resuscitation of the burned patient Emerg Med J 2003;20:109 doi:10.1136/emj.20.1.109
- London and South East Burns Network Burns Referral Guidelines: criteria for referral 2015
- New Zealand National Burn Service, Escharotomy Guidelines
- British Burns Association (2016), “Emergency Management of Severe Burns 16th ed.”
- Public Health England. Tetanus: the green book, chapter 30, 2013. Last updated 2020.
- Dollery W., Cardiac monitoring not needed in household electrical injury if the patient is asymptomatic and has a normal ECG. BestBETs, 2000






18 Comments
Very Useful, Thank you
very useful
sums up initial management of burns in A&E
Excellent review of topic thanks
Excellent review.Thanks.
Really excellent-thank you
very useful , thanks.
Brilliant. Thanks
good revision of burns
Escharotomy can be life saving
Very informative, thank you
Really useful module highlighting the appropriate assessment and prompt management of burns in the ED.
Great learning module for someone with limited burns’ exposure.
Thank you. V helpful resource
excellent revision
Very good presentation of burns in pediatrics. Thank you.
Easy to comprehend and very helpful.
Nice fruitful topic
very helpful for updating my knowledge