Authors: Madeline Payne / Editor: Charlotte Davies / Codes: ObP2, ObP6, SLO1, SLO3 / Published: 24/05/2022
We have a reluctance to perform speculum and vaginal examinations in the ED, despite the “lost condom” being a regular MRCEM OSCE station. Many times our hesitancy is justifiable, but here are a few considerations for why ED practitioners should all be comfortable at performing speculum examinations and bimanual examinations. It could be life saving.
BEFORE: WHEN TO CONSIDER VAGINAL EXAMINATION IN ED
No-one likes a speculum or bimanual examination, doctors included, but sometimes you just have to accept the inevitable. As a general rule, as with anything else, it’s going to be worth doing if it will change immediate management, fix the problem completely or help to stabilise the patient.

Cervical shock
Cervical stimulation or stretching can produce a vasovagal response with bradycardia and hypotension. If the stimulation is not removed, this can cause circulatory compromise. As it requires something to be in the os of the cervix, rather than in the canal, the most common scenario would be during a miscarriage with products of conception getting stuck.
Heavy PV bleeding in pregnancy with haemodynamic instability
Late term miscarriages are more likely to bleed heavily, as are patients on anticoagulation (unsurprisingly). If a patient is bleeding heavily and is beginning to decompensate, you may be able to stop/slow the bleeding if you’re able to remove clots and any visible products of conception which will cause ongoing bleeding until removed.
Foreign bodies
The classic PV FB would be a stuck tampon or condom, although as with rectal FBs you never quite know… The first thing to consider is that there’s a decent chance it’s not there, and the patient will usually have already had a good feel, with ED likely to be their absolute last resort. If they haven’t tried to remove it themselves for whatever reason, you could consider asking them to go to the patient toilet themselves and having a go, with reassurance that this is safe.
WHEN NOT TO DO A SPECULUM
- If you do not feel confident/comfortable performing a speculum examination
- If the patient doesn’t consent
- If there is any question of sexual assault that may require forensic evidence to be taken (unless the patient is unstable and it is clinically indicated)
WHAT YOU NEED
- Lube – lots of lube!
- PPE (especially gloves)
- Speculum
- The specula in ED are generally the single use plastic double-bladed ones – make sure you know how to open the speculum and how to screw it open before going anywhere near the patient (it’s not terribly reassuring for the patient if you have to stop halfway through to mess around and work out how to use the equipment)

- They most commonly come in three sizes (although only medium may be available) – the medium size should be fine for the majority of women.
- The specula in ED are generally the single use plastic double-bladed ones – make sure you know how to open the speculum and how to screw it open before going anywhere near the patient (it’s not terribly reassuring for the patient if you have to stop halfway through to mess around and work out how to use the equipment)

- Forceps
- Preferably polyp/sponge holding forceps as they have a wider end, or long Spencer Wells artery forceps also work – anything long with interlocking handles.

- Preferably polyp/sponge holding forceps as they have a wider end, or long Spencer Wells artery forceps also work – anything long with interlocking handles.
- Light source
- Ideally a lamp but pen torch will do
- Specimen pot
- You’ll need something to put any products of conception or foreign bodies into if removed
- Lots of gauze
- Paper towels to clean up after
- ?swabs
- If you’re thinking infected retained tampon and you’re doing the speculum exam anyway, you might consider doing a high vaginal swab (usually the same swabs as wound swabs) to send for MCS
- If the patient is concerned about STIs, they should really be re-directed to local sexual health services instead
- Chaperone
- Preferably female
- Make sure you explain what you’re going to do to your chaperone as well – it’s hard to re-direct the light source or open the swabs yourself once you’ve started examining, so having someone who knows what they’re doing or who has done specula before themself is a bonus
PREPARING THE PATIENT
- Ideally, any intimate examination would be done in a private room (preferably with a lock!) but we all know that that’s a challenging prospect in ED
- If you have to use a cubicle, one top tip is to turn the trolley around so that the patient’s head is towards the entrance – that way if you’re interrupted, at least some of their dignity is preserved.
- Make sure you explain what you’re going to do very carefully before you go anywhere near the patient, including digital examination if you’re planning to do this.
- Make sure you know whether they’re pregnant or not.
- Don’t assume they have had a speculum examination before, and remember that there’s a lot of stigma/horror stories about vaginal examination so lots of reassurance may be needed.
- Once the patient has consented to the examination, ask them to remove their bottoms and underwear and lie on the bed (covered with the second sheet), and leave the room to give them some privacy.
- Make sure they’ve been to the loo if needed.
- Make sure the second sheet is covering them as much as possible too, particularly while still preparing your equipment.
- If you’re anticipating any bleeding/discharge/removal of objects, put an inco pad under the patient and have some more handy.

DURING
HOW
- Positioning
- Put the trolley up to a height that’s comfortable for you and your back, and make sure you can stand on the side of the patient that corresponds to your dominant side (ie. if you’re left handed and will be holding the speculum in your left hand, stand on the patient’s left
- Ask the patient to lie flat (or as flat as able), with the back of the bed/trolley down
- Ask them to bend their knees as much as possible, and keep their feet together
- Once the knees are bent, get them to open the legs whilst keeping their feet together and drawn as far up as possible
- It’s easiest to explain it as something like “bring your feet up to your bum as far as possible and then let your knees flop open”
- Basic speculum technique
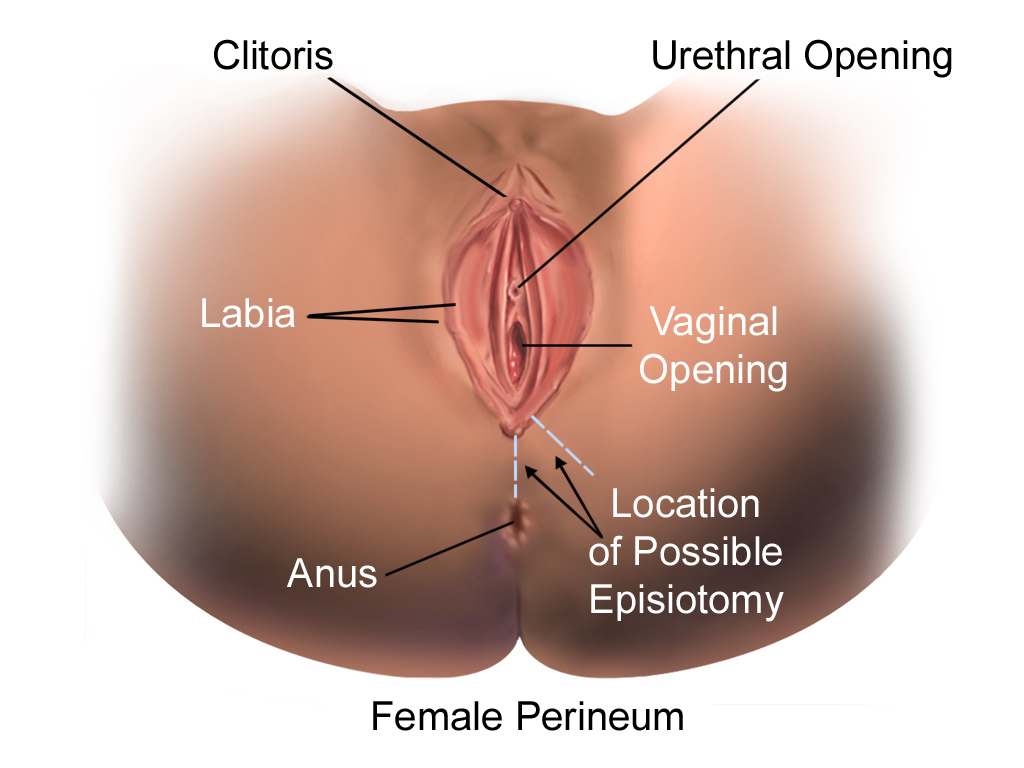
- Start with external examination, including any signs of FGM (female genital mutilation), any ulcers or any other abnormalities
- Gently part the labia with your non-dominant hand and insert the speculum closed with the blades perpendicular to the bed using your dominant hand.
- Once inserted, turn the speculum so the handle is pointing up and the blades are parallel to the bed
- Reassure the patient and encourage relaxing breathing and relaxation if needed.
- Slowly open the speculum (make sure you warn the patient first!) and adjust until the cervix is visible and central
- Turn the screw on the speculum clockwise until the blade position is fixed – this will free up the dominant hand if needing to remove things
- Once you’re done, SLOWLY loosen the screw holding the speculum open and gradually withdraw. If you close the speculum too quickly, it’s very easy to catch the cervix between the blades which is incredibly uncomfortable for the patient.
- This is summarised well on Geeky Medics.
- What you might see
- Cervix should be smooth, os may be round or slit depending on parity

- Cervix should be smooth, os may be round or slit depending on parity
-
- Other stuff you may see:
- Ectropion
- This is the spread of the inner cervical epithelium to the external cervix. It looks like a redder rougher area around the os, and may bleed on contact.
- Ectropion is common and benign. It is more likely in women on hormonal contraception, who are pregnant, or who are closer to menarche.
- Coil strings
- These are to be expected if someone has an IUD in – if you can’t see them and the patient has told you they have a coil, they will need to see a GP/GUM clinic for a coil check
- They look like bits of wire coming from the os – usually there will be two
- Colour can vary but is generally white or black.
- Discharge
- Discharge is normal! Everyone will have some physiological discharge, which is usually whitish or pale yellow
- Other discharge differentials:
- Smelly/watery/grey: bacterial vaginosis
- Thick/lumpy/”cottage cheese”: vaginal candidiasis/thrush
- Purulent, especially around os: cervicitis (chlamydial or gonorrhoeal)
- Smelly/brown/excessive in the context of retained foreign body: likely to be infected
- Anything else: if you have any concerns or just aren’t sure what you’re seeing, advise the patient to see their GP or consider referring to colposcopy/2WW depending on local protocols and the specific case context
- Ectropion
- Other stuff you may see:
WHAT TO DO
- Removal of objects
-
- Make sure you get a good view of the whole vagina, including the cervix and the posterior fornix (the bit under/behind the cervix)
- If you have a clear view of what you’re trying to remove, you can just grab it with forceps and gently pull it out.
- If they have an IUD in, try not to pull it out.
- If there is a retained tampon (or any other object that’s been there a while), be prepared for the smell…
- Heavy bleeding
- If there’s a lot of clots obscuring the view of the cervix, you can remove any clots in the canal with forceps and gauze to get a good look at the cervix.
- If anything looks like tissue (more rough texture, anything that doesn’t just look like blood), try and remove separately into a histology pot.
- If the clots are large, gently pull them out with the forceps (they’ll break if you try to grab them)
- Remember to try and keep track of clots/blood removed for an overall estimated blood loss figure.
- Products of conception
- If you can see anything that looks like POC, be as gentle as possible in pulling out the tissue – if it breaks and part is retained in the cervix or uterus, you may cause more issues
- If POC is stuck in the cervix and the patient has signs of cervical shock, try and gently pull it out without further cervical stimulation – this might be hard, and may require an urgent call to gynae if the patient is decompensating
- You can also try sweeping the cervix with gauze to see if that helps move things
- Digital examination for foreign bodies
- If you’re unable to visualise a foreign body but have a high level of concern that something is there, you can do a bimanual/digital exam (EPV)
- In a patient who is very anxious or who hasn’t been sexually active, this may also be more comfortable as the initial port of call, although it obviously doesn’t allow for visualisation
- Put on sterile gloves, and apply plenty of lube to the first two fingers of your dominant hand
- Gently insert two fingers into the vagina and feel for the cervix
- Feel around cervix and sweep the fornices for any objects. Note any cervical excitation (very tender cervix) or adnexal tenderness which could point to PID
- For a full bimanual, perform abdominal palpation at the same time and feel for adnexal masses or tenderness – probably not strictly necessary if you’re just trying to remove an object
GENERAL TIPS
- If you’re struggling to visualise the cervix, ask the patient to make a fist with both hands and put them in the small of their back – this should tilt the pelvis and can bring the cervix into view
- A classic tactic is to ask the patient to cough as you’re putting the speculum in as it can help the pelvic muscles relax and make it more comfortable for the patient. Asking the patient to cough and therefore increase intraabdominal pressure can also sometimes help with expelling clots or POC.
- Make sure you’re comfortable – check the bed is high enough and that you’re standing on the side of the patient that will allow you to use your dominant hand.
AFTER
Antibiotics
A check of the BASHH guidelines and even a general Google search doesn’t actually give a definitive answer on when to give antibiotics following a vaginal retained foreign body. If there is any evidence of infection (excessive discharge, smell, fever, abdominal pain etc.), the consensus seems to be to give antibiotics, probably something with broad cover like co-amoxiclav. Any patients with retained foreign bodies should be safety netted regarding infection.
GUM/sexual health follow up
If a patient has had a retained condom, they should be managed as someone who has had unprotected sexual intercourse, including a risk assessment for PEPSE and any need for emergency contraception. They should also be advised to have an STI screen, and safety netted for signs of STIs, as well as infection secondary to the retained condom.
Bleeding
Heavy bleeding should improve with clot removal if the os is closed – if the os is still open, gynae referral may be appropriate as this indicates ongoing miscarriage. If the os is closed and patient stable, you may be able to discharge with Early Pregnancy or equivalent follow up.
Handling of products of conception
Products of conception are defined as any tissue that has developed from a pregnancy. Different hospitals have different guidance and regulations regarding management and disposal of POC. Legally, this is managed by the Human Tissue Authority, which states that a conversation must be had with the patient and carefully documented regarding disposal of remains (as long as the pregnancy did not progress past 24/40) and consent for any histological examination of POC as per local protocols. There may be forms or hospital-specific rules on this (e.g. a specific form to be filled in with consent for histological examination followed by communal cremation of remains).
WHAT TO INCLUDE IN A GYNAE REFERRAL
- Parity – in the form Gx Py where G is gravidity (number of pregnancies including any current) and P is parity (number of live births). Bonus marks for giving method of delivery for any children and outcomes of any other pregnancies.
- Basic gynae history including last menstrual period (LMP), last smear test if eligible and any history of abnormal smears, and any contraception being used
- Indications for admission that they might consider:
- Is the os open – this is one of the most important questions as it will guide management, but unfortunately can be hard to answer, particularly if you don’t do speculum examinations very often
- Is the patient haemodynamically stable – are they tachycardic/hypotensive/have there been any syncopal/pre-syncopal episodes?
- Has the Hb dropped?
- Is there ongoing bleeding or severe pain?
- Unless a patient is unwell/you’re suspecting PID or TSS, most patients who have had a foreign body removed shouldn’t need to see gynae.
Hopefully that’s provided some useful tips and suggestions for you. Add your tips in the comments!
For more RCEMLearning gynae content why not visit our induction module on gynae and bleeding in early pregnancy, and the linked sessions for ObP1 – ObP7 and ObC1 – ObC19 on the syllabus page.
References
- Female perineum. Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). Wikimedia Commons.
- Cervix birth. CFCF. Wikimedia Commons, 2014.




4 Comments
Amazing module, was easy to follow with good illustrative summary points…
Helpful topic in emergency settings
Really helpful and concise module
Good summary with some fantastic tip for the non-gynae EM doctor.