Author: Jules Blackham, Jason M Kendall, Roland Watura / Editor: Jason B Lee / Reviewer: Emma Everett, Joe Schrieber / Codes: ELP3, MuP3, SLO2, SLO4, TP2 / Published: 11/10/2021
Cervical spine injuries are rare but potentially devastating. Historically Immobilisation of the cervical spine on the slightest suspicion of injury is recommended by most resuscitation courses including ALS, ATLS, APLS, PHTLS, as well as by NICE and JRCALC (National Ambulance Service Guidelines). To that end, cervical spine immobilisation was previously the most commonly performed procedure in pre-hospital care.23
According to NICE guideline,21 on assessment, maintain In-line manual immobilisation when assessing/instrumenting the airway.
At all stages, protect the spine and avoid moving the remainder of the spine.
Assess the person for spinal injury, initially taking into account the factors listed below. Immobilise if any of:
- has any significant distracting injuries
- is under the influence of drugs or alcohol
- is confused or uncooperative
- has a reduced level of consciousness
- has any spinal pain
- has any hand or foot weakness (motor assessment)
- has altered or absent sensation in the hands or feet (sensory assessment)
- has priapism (unconscious or exposed male)
- has a history of past spinal problems, including previous spinal surgery or conditions that predispose to instability of the spine.
In a review of the literature (209,320 patients) evaluating the potential for cervical spine injury in a trauma population, Milby et al. found that the overall incidence of actual cervical spine Injury was 3.7%. In alert patients the incidence was only 2.8%, whilst those who were clinically unevaluable (because of depressed conscious level, intoxication, etc) there was a higher incidence of 7.7%. This means that, in patients who present to hospital with potential neck injuries, the vast majority of them will not actually subsequently be shown to have a cervical spine injury.
Cervical spine immobilisation is not a benign procedure:
- Collars significantly raise intracranial pressure: an effect that is potentially significant in the presence of head injury
- Long boards and collars cause pain and tissue ischaemia which can lead to pressure sores
- Supine immobilisation causes considerable deterioration in respiratory function
A large number of patients present to Emergency Departments (ED) with their necks immobilised; as significant cervical spine injury is rare and there are potentially adverse consequences of cervical spine immobilisation, reliable methods are needed to clinically exclude cervical spine injury wherever possible (‘clearing their necks’). The initial clinical assessment and, where necessary, subsequent radiological assessment, of potential cervical spine injury is the subject of this session.
Learning Bite
Cervical spine immobilisation is not a benign intervention. It is associated with significant morbidity.
(a) Anatomy
Bony components:
- Vertebral body which gives the vertebrae its strength and weight bearing ability
- Vertebral arch formed by Pedicles and laminae which with the vertebral body form the vertebral foramen
- Vertebral foramen align to from the vertebral canal for the spinal cord
- Seven processes:
- Spinous process projects posteriorly from the vertebral arch
- Two transverse processes posterolaterally from intersection of pedicles and laminae; the spinous and transverse processes allow attachment of the deep muscles of the back
- Four articular processes two superior and two inferior to articulate with vertebrae above and below in the articular facet joints
Ligamentous components:
- The anterior longitudinal ligament
- Strong broad fibrous band which covers the anterior of the vertebral bodies and intervertebral discs and which extends from pelvic surface of sacrum to anterior tubercle of C1 vertebra
- Maintains stability of intervertebral joints and prevents hyperextension of vertebral column
- The posterior longitudinal ligament
- Narrower and weaker fibrous band which runs within the vertebral canal along the posterior aspects of vertebral bodies from C2 to sacrum
- Helps prevents hyperflexion of vertebral column and protrusion of intervertebral discs
- The Ligamentum flavum
- Joins laminae of adjacent vertebral arches that extends from vertebrae above to vertebrae below and which binds the laminae of adjacent vertebrae together and forms part of posterior of vertebral canal
- Resists separation of vertebral laminae and so attempts to prevent abrupt flexion of vertebral column
- The Interspinous and supraspinous ligaments
- Adjacent vertebrae joined by weak interspinous and strong supraspinous ligaments; the supraspinous ligament merges with nucal ligament in the neck
- The Intertransverse ligaments
- Connect adjacent transverse processes with scattered fibres in cervical spine, becoming stronger in thoracic spine
(b) Mechanism of injury
Abnormal flexion, extension, rotation and compression cause injury to the spine in predictable ways.3 As described below, the ligaments of the neck can be injured from all of these mechanisms. The lesser forms of these injuries may cause injuries to the ligaments without the associated fractures. All injuries to the neck have the potential to damage the spinal cord. This can present as weakness or altered sensations in nerve root distributions or in incomplete spinal cord injury patterns (e.g. central cervical cord syndrome or Brown-Sequard syndrome). Clearly patients with neurology will all require specialist imaging (e.g. CT and/or MRI) and referral for further care and so will not be discussed further in this session.
Hyperflexion
Hyperflexion causes compression of the anterior aspects of the vertebral bodies and posterior ligament complex distraction. This leads to:
- Chance fractures
A chance fracture is a horizontal fracture through the body, pedicle and posterior elements of the vertebrae.
Tear drop fractures
A tear drop fracture is a fracture of the anterior superior corner of inferior vertebrae. (see Figure 1)
- Rupture of posterior ligament
- Odontoid peg
The odontoid peg may also be fractured by sudden severe flexion (see Figure 2)
Figure 1: Tear Drop Fracture
Figure 2: Odontoid Peg Fracture
Flexion and rotation
- 50%-80% of cervical spine injuries are caused by this mechanism as are most thoracolumbar injuries
- This mechanism causes disruption of the posterior ligament complex and the posterior column
- The facet joints, lamina, transverse processes, and vertebral bodies may fracture
- Relatively flat facet joints may dislocate without fracture
- Spinous processes of C6/7 can also be avulsed by interspinous ligaments the so-called clay-shovellers fracture
- All intervertebral ligaments may tear and the upper vertebral body can be displaced relative to the one below
Hyperextension
- Damages the anterior column
- This is associated with anterior fracture of the anterior inferior aspect of vertebral body
- The posterior aspect of the vertebral body may be crushed with a risk of retropulsion of bony fragments or the intervertebral disc into the spinal canal
- Hangmans fracture (see Figure 3): hyperextension fracture through pedicles of C2 following hyperextension with distraction or compression. Results from judicial hanging (rather than suicidal which causes asphyxiation) or from striking chin on steering wheel in a collision.
Figure 3: Hangmans fracture
Rotation
- Rarely occurs in isolation
- Primary injury occurs to the posterior ligament complexes, and is often unstable
- May result in facet joint dislocation (see Figure 4)
Figure 4: Facet joint dislocation (see slippage of C4 on C5):

Compression
- This mechanism is common in thoracic and lumbar spine injuries and results in wedge fractures
- The Jefferson Fracture of C1 (see Figures 5 and 6) is a specific cervical spine fracture caused by an axial loading mechanism (eg. a weight landing on patients head, or patient landing on their head after a fall).
The characteristic features are:
- The atlas is compressed between the occipital condyle and C2
- The laminae and pedicles are fractured and transverse ligament holding peg in position can be torn.
- The skull and C1 may slide forward on C2.
- There can be significant shift before compression of spinal cord occurs as 1/3rd of the space of the spinal canal is occupied by the odontoid peg, 1/3rd by areolar tissue and 1/3rd by the spinal cord itself.
Figure 5: Jefferson fracture (note overriding of the lateral masses of C1 on C2)
Figure 6: CT Images of Jefferson # (Different patients scan)
(c) Differences between adults and children (4)
The anatomy and relationships of the childs cervical spine is different to that in adults:
- Children have relatively larger heads
- Their ligaments and joint capsules are more lax
- Their facet joints are more horizontal
- Their vertebral bodes are wedge shaped
This has the following consequences: (a) Pseudosubluxation refers to the appearance of forward slippage of one vertebral body on another (see figure 7); pseudosubluxation of C2 on C3 occurs in 24% of under 8 year olds and of C3 on C4 in14% of under 8 year olds. (b) SCIWORA (Spinal Cord Injury without radiological abnormality) which is defined as objective signs of myelopathy as a result of trauma with no evidence of fracture or ligamentous instability on plain radiographs or tomography. It is more common in children and is reported to occur in up to 30% of spinal cord injuries in children. Younger children below 10 yrs are also more likely than older children to:
- Injure the upper cervical spine (C1-C4) compared with lower c-spine
- Dislocate the cervical spine
- Injure the spinal cord itself
The cervical spine takes on its adult form from about the age of 8 years.
Figure 7: Pseudosubluxation (note the apparent forward slippage of C2 on C3)
Learning Bite
The cervical spine in children is anatomically different to that in adults and this results in different patterns of injury.
Clinical Assessment: Adults
For the purposes of clearing the cervical spine, patients can be divided into two groups:
- Conscious cooperative patients: This is the most commonly encountered group of patients who present to the ED or pre-hospital practitioner. They have a low incidence (less than 3%) of cervical spine injury and are able to cooperate with clinical assessment. Therefore, a focussed history and examination can be used to clinically clear their necks – various clinical decision rules have been developed to be used in these patients:
- NEXUS Low Risk Criteria
- Canadian Cervical Spine Rules
- Unconscious/uncooperative patients: These patients are not able to have their cervical spines cleared clinically as a reliable clinical assessment cannot be made. These patients require imaging to clear their spines
NEXUS Low Risk Criteria (NLC) [5]
This was developed from a prospective study of patients undergoing cervical spine radiography in 21 centres in the USA. The study looked at 5 criteria; if all were negative the patient was classified as having a low risk of injury.
Five NEXUS criteria:
- No midline cervical tenderness
- No focal neurological deficit
- Normal alertness
- No intoxication
- No painful distracting injury
A total of 34,069 patients underwent radiography, and all but 8 of 818 patients with cervical spine injury were identified by applying the NEXUS criteria (a sensitivity of 99%; 95% confidence intervals 98.0-99.6%). The negative predictive value was 99.8%, but the specificity was low (12.9%) which means that the majority of patients with positive NEXUS criteria still did not have actual cervical spine injury. Some authors have tried to refine the NEXUS Guidelines without success.
Canadian C-Spine Rule (CCR) [6]
It should be noted that, due to reduced radiation and increased availability, there is increasing utility of CT as first line imaging modality in the over 65yo population (due to difficulty in interpreting plain radiographs). Please review individual trusts local policy.
This prospective cohort study in 10 Canadian EDs evaluated 20 standardised clinical factors prior to radiography in 8924 patients. The study sample included 151 (1.7%) clinically significant cervical spine injuries. The decision rule resulting from this study asks three questions:
- Is there any high-risk factor present which mandates radiography?
- Is there any low-risk factor present that allows safe assessment of the range of neck motion?
- Is the patient able to actively rotate their neck 45º to the left and right?
Subsequent validation of this rule revealed a sensitivity of 100% (95% confidence intervals 98-100%) and a specificity of 42.5% (95% confidence intervals 40-44%).
Unlike the NEXUS rule, this study excluded children <16 yrs of age, and all patients with a Glasgow Coma Scale (GCS) score of <15.
CCR or NLC?
There have been two studies which have compared the CCR with the NLC. Both these studies found that the CCR had a higher sensitivity and specificity than the NLC, however one study was a retrospective application of the NEXUS criteria to the CCR study raw data, and did not exactly follow the NEXUS criteria (No evidence of intoxication vs. unevaluable due to intoxication).
the most recent NICE guidance (2016) advises clinical assessment utilising the Canadian C-spine rules.
The CCR are used more in EDs in the UK at present (anecdotal), and the NLC are currently used in the pre-hospital setting being recommended by the current JRCALC (national ambulance service) Guidelines. However a number of ambulance services are now training their staff in the use of the CCR.
Learning bite
The cervical spine can reliably be ‘cleared’ if either the NEXUS low risk criteria or Canadian C-Spine rules are satisfied
Clinical Assessment: Children
Childrens cervical spines are different to those of adults (see above), with injury to the upper cervical spine and purely ligamentous injury being more common. In addition, younger children are often harder to assess being frightened and uncooperative.
Clinical exclusion of cervical spine injury in children:
Viccellio and colleagues9 performed a subgroup analysis of the NEXUS study, specifically evaluating children with neck injury. This group consisted of 3,065 children aged under 18 of whom 30 (0.98%) sustained a cervical spine injury. This incidence is lower than that in the adult population, but this may have be due to more liberal use of radiography in children. There were no children with proven spine injury who were negative on all five NEXUS criteria, and no cases of SCIWORA. 45.9% of injuries occurred in the lower cervical spine (C5-C7). There was no spinal injury in children under 2 years and only 4 cases in children under 8 years of age in this study population, which means that, despite its apparently impressive performance, the NEXUS rule should be used with caution in these younger age groups.
A recent study compared the NLC and CCR in children10. The study evaluated children less than 10 year of age, who had radiographs of their cervical spine over a 10 year period. Of the 125 children who had radiographs, 7 (3%) had clinically significant fractures. If the NLC was applied 3 fractures would have been missed (sensitivity=43%, specificity =96%) whereas the CCR would have missed 1 fracture (sensitivity=86% and specificity=94%). They concluded that, although the CCR performed better than NLC, neither could be used with confidence in children.
Clinical bottom line: There is no robust evidence base for a clinical rule-out for cervical spine injury in children less than 10 years of age.
Patients, whose cervical spine cannot be clinically cleared, will require imaging to permit identification or exclusion of significant injury.
(a) Plain cervical spine series
Plain radiographs do not detect all cervical spine fractures. In 29 published studies 16% of fractures (range 0 to 67%) were missed11. Plain lateral X-rays alone have a sensitivity of 63-85%, while the three view trauma series (anterior-posterior (AP), lateral and peg views) improved diagnostic sensitivity to over 93%. Plain radiographs are not adequate to exclude significant cervical spine injury in unconscious patients and these patients will require CT (or MRI) imaging (see below).
Normal imaging of the cervical spine consists of three views (see Figure 8). The Lateral, Antero-posterior (AP) and odontoid peg views.
In children under 5, the PEG view is considered unnecessary12.
(i) Lateral film
- Adequacy Visible base of skull to top of body of T1
- Alignment:
- Along anterior margins of vertebral bodies
- Posterior margins of vertebral bodies
- Bases of spinous processes
- Bone inspection of vertebral bodies
- Intervertebral discs- uniform height
- Soft tissues:
- C1-4 max of 7mm (30% of vertebral body width)
- C5-7 max of 22mm (100% of vertebral body width)
- PEG anterior arch of C1 no more than 3mm in adults (5mm in children) space between anterior arch of C1 and PEG
(ii) AP View
- Spinous processes should be in a straight line except if bifid spinous process
- Distance between spinous processes approximately equal
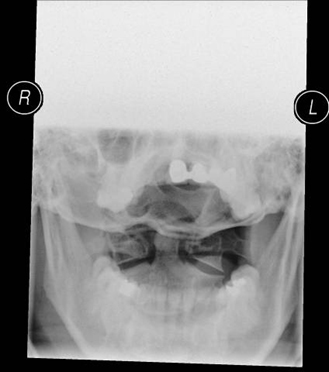
(iii) Odontoid Peg View
- Lateral margins of C1 should lie within lateral margins of C2
- Spaces on each side of peg should be equal slight variation if neck is slightly rotated
Figure 8: Normal series of plain cervical spine x-rays
(i) Lateral view:
(ii) AP view:
(iii) Otonoid peg view:
(b) Swimmers view (see Figures 9 and 10):
In the case of an inadequate lateral view:
- an arm pull view in which the patients arms are pulled down to try to lower the shoulders so the lower cervical spine can be visualised or
- a Swimmers view is obtained in which the arm nearest the x-ray machine is elevated and the arm nearest the plate is kept extended. This view can be difficult to interpret due to overlying bones.
Figure 9: Position for swimmers view
Figure 10(a): Inadequate plain lateral x-ray
Figure 10(b): Swimmers view now demonstrating C7/T1
(c) Flexion / extension views
For many years flexion/extension views used to be recommended for the clearing of the cervical spine. A number of studies have demonstrated flexion/extension views find fractures with may not be visible on initial plain films, although these fractures are invariably visible on CT. In a review of the NEXUS study data13 86 of the 818 patients with cervical spine injuries had flexion/extension views. Four dislocations and 15 out of 16 subluxations were seen. However, all the dislocations and all but four of the subluxations were visible on plain films. These four patients had significant injuries of the c-spine, such that subsequent imaging would have shown these injuries. Other studies have demonstrated that flexion/extension views may find injuries which are not visible on plain films, however these patients are either intoxicated or have significant neck pain and the injuries were apparent of CT. Flexion/extension views should not be performed on unconscious / uncooperative patients as there have been cases of paraplegia following this procedure.
Learning Bite
Clinical bottom line: There is no role for flexion/extension views in the acutely injured neck.
(d) Computerised Tomography (CT)
It has been recommended that thin cut axial CT scans with sagittal reconstruction should be used to view areas that were suspicious or poorly visualized on plain radiographs14. However, the indication for CT scanning needs to be carefully considered because patients undergoing CT of their whole cervical spine have a 14-fold increase in the dose of radiation to their thyroid gland compared with standard three view plain radiography.
The recent introduction of spiral CT has reduced radiation dose and is faster, with a reported sensitivity as high as 99% and a specificity of over 93%15. The missed injuries are normally ligamentous, and may only be detected with Magnetic Resonance Imaging (MRI) or flexion/extension views. There are well documented cases of conscious and cooperative patients with normal plain films and normal CT scans who were subsequently found to have unstable ligamentous injury on MRI scanning.
(e) Magnetic Resonance Imaging (MRI)
MRI scanning is very sensitive for soft tissue injuries including ligament injuries, disc herniation and haemorrhage, which are less well visualised on CT.16 Many of these injuries will not be clinically significant, but a minority will represent unstable injuries. MRI is, however, less sensitive than CT at imaging the posterior elements of the spine and the craniocervical junction.
MRI is indicated if there is any neurology referable from the cervical spine, or if there is severe pain, despite a normal CT scan as some unstable ligamentous injuries may only be seen on MRI
CT vs. MRI scanning
In unconscious patients there is some concern about the possibility of ligamentous instability which may be missed by CT, and so some authors consider that patients should have MRI to clear the spine in these patients. Isolated ligamentous injury in the cervical spine is rare (0.04% incidence of ligamentous injury without fracture17). The incidence in patients with altered mental state is higher, but is still only 0.7%. MRI in an unconscious polytrauma patient is not straightforward, and in many patients may not be practical for many days.
The current NICE Guidelines do not recommend that MRI is routinely used to clear the cervical spine. The EAST guidelines from the USA are non-committal, leaving the decision to use MRI up to the individual hospital.
Learning Bite
Current NICE Guidelines do not recommend the routine use of MRI scanning to clear the cervical spine.
Adults
1.5.6 Perform CT in adults (16 or over) if:
imaging for cervical spine injury is indicated by the Canadian C-spine rule (see recommendation 1.4.7) or there is a strong suspicion of thoracic or lumbosacral spine injury associated with abnormal neurological signs or symptoms.
1.5.7 If, after CT, there is a neurological abnormality which could be attributable to spinal cord injury, perform MRI.
1.5.8 For imaging in adults (16 or over) with head injury and suspected cervical spine injury, follow the recommendations in section 1.5 of the NICE guideline on head injury.
Children
1.5.2 Perform MRI for children (under 16s) if there is a strong suspicion of:
cervical spinal cord injury as indicated by the Canadian C-spine rule and by clinical assessment or cervical spinal column injury as indicated by clinical assessment or abnormal neurological signs or symptoms, or both.
1.5.3 Consider plain X-rays in children (under 16s) who do not fulfil the criteria for MRI in recommendation 1.5.2 but clinical suspicion remains after repeated clinical assessment.
1.5.4 Discuss the findings of the plain X-rays with a consultant radiologist and perform further imaging if needed. Spinal injury: assessment and initial management (NG41)
NICE 2016. All rights reserved. Page 12 of 23
1.5.5 For imaging in children (under 16s) with head injury and suspected cervical spine injury, follow the recommendations in section 1.5 of the NICE guideline on head injury.
Above guidelines are from NICE February 2016 Spinal Injury: Assessment and Initial Management
CT as primary imaging modality
- GCS below 13 on initial assessment
- Patient has been intubated
- Plain film series is technically inadequate (eg. desired view unavailable), suspicious or definitely abnormal
- Continued clinical suspicion of injury despite a normal X-ray
- The patient is being scanned for multi-region trauma
The current Eastern Association for the Surgery of Trauma (EAST) Guidelines18 from the USA recommend CT as the primary imaging modality for all patients who require their cervical spine imaging.
Historically there has been controversy about how to manage simple neck sprain injury (i.e. injury to the neck where there has been no demonstrable bony injury or unstable ligamentous injury) and there have been few trials evaluating specific interventions.
A Cochrane review in 200719 reviewed the evidence for conservative management of neck sprain injury (so-called whiplash ). They found that there was insufficient evidence to support or refute the effectiveness of active versus passive treatments to relieve the symptoms of neck sprain injury. There were, however, a number of trials in this review which reported that cervical spine collars resulted in worse outcome than early mobilisation.
Although there are no randomised trials evaluating the use of analgesia in the management of neck sprain injury, it would be sensible to recommend analgesia to permit early mobilisation.
Patients who have a spinal cord injury should remain immobilised and immediately be discussed with the nearest Neurosurgeon or Spinal Surgeon on call by the trauma team leader or senior doctor in charge of the patient’s care.
There is considerable uncertainty surrounding the prognosis from neck sprain injuries. It is clear that the vast majority of patients have a good prognosis, however certain risk factors predicting worse prognosis have been reported20:
- Older age
- Female gender
- Baseline neck pain and headache intensity
- Baseline radicular signs/symptoms
Insurance and compensation claims have been found to be associated with a worse prognosis. In countries without a litigation culture the prognosis of neck sprain injury is considerably better that in countries with a more litigious system. Regardless of the legal system it has been noted that instruction of a lawyer shortly after a collision is independently associated with slower recovery.
- The elderly are at high risk of cervical spine injury from relatively minor mechanisms of injury (e.g. falling from standing): always consider the possibility of a neck injury in an old patient with a fall and head injury.
- Missed cervical spine fractures tend to occur in patients with distracting injuries, reduced level of consciousness or under the influence of alcohol or drugs.
- If the patient is holding their neck in a flexed position, DO NOT try to get into a collar. There are many case reports of paralysis resulting from putting patients with Ankylosing Spondylitis into a collar.
- Cervical spine injuries are uncommon, but spinal immobilisation is very commonly performed
- Cervical spine immobilisation is not a benign intervention and should be removed as soon as is safe and practicable after trauma (Level of evidence C)
- In the conscious co-operative patient, radiological imaging of the cervical spine is NOT required if either the NEXUS Low Risk Criteria or the Canadian C-Spine rules are satisfied (Level of evidence B)
- If significant clinical concern remains after normal plain radiographs, CT should be considered as a second modality of imaging due to the low sensitivity of plain radiographs
- The cervical spine can be cleared with a normal CT (with saggital and coronal reconstructions) (Level of evidence C)
- In the unconscious patient plain radiographs add nothing to CT and should not be performed (Level of evidence B)
- Flexion / Extension views should not be performed in the acutely injured patient (Level of evidence B)
- The cervical spine can be cleared with a normal MRI (Level of evidence B)
- Milby AH, Halpern CH, Guo W, et al. Prevalence of cervical spinal injury in trauma. Neurosurgical Focus 2008;25(5):E10.
- Benger J, Blackham J. ”Why do we put cervical collars on conscious trauma patients?” Scand J Trauma Resusc Emerg Med 2009;17:44.
- Greaves I, Porter K, Garner J. Trauma Care Manual. 2nd edn. Hodder and Arnold, 2009. Chapter 12.
- Slack SE, Clancy MJ. Clearing the cervical spine of paediatric trauma patients. Emerg Med J 2004;21:189-193.
- Hoffman JR, Mower WR, Wolfson AB et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med 2001;343:94-9.
- Stiell IG, Wells GA, Vandemheen KL et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 2001;286(15):1841-8.
- Dickinson G, Stiell IG, Schull M et al. Retrospective application of the NEXUS low-risk criteria for cervical spine radiography in Canadian emergency departments. Ann Emerg Med 2004;43(4):507-14.
- Stiell IG, Clement CM, McKnight RD et al. The Canadian C-Spine Rule versus the NEXUS Low-Risk Criteria in Patients with Trauma. N Engl J Med 2003;349:2510-2518.
- Viccellio P, Simon H, Pressman BD et al. A Prospective Multicenter Study of Cervical Spine Injury in Children. Pediatrics 2001;108:e20-20.
- Ehrlich PF, Wee C, Drongowski R et al. Canadian C-spine Rule and the National Emergency X-Radiography Utilization Low-Risk Criteria for C-spine radiography in young trauma patients. Journal of Pediatric Surgery 2009;44(5):987-691.
- Blackham J, Benger J. Clearing the cervical spine in conscious trauma patients. Trauma 2009;11(2):93-109.
- Swischuk LE, John SD, Hendrick EP. Is the open-mouth odontoid view necessary in children under 5 years? Pediatric Radiology 2000;30:186-189.
- Pollack CV Jr, Hendey GW, Martin DR et al. Use of flexion-extension radiographs of the cervical spine in blunt trauma. Annals of Emergency Medicine 2001;38(1):8-11.
- Marion DW, Domeier R, Dunham CM et al. Practice management guidelines for identifying cervical spine injuries following trauma – Update EAST Practice Parameter Workgroup for Cervical Spine Clearance 2001.
- Ptak T, Kihiczak D, Lawrason JN et al. Screening for cervical spine trauma with helical CT: Experience with 676 cases. Emergency Radiology 2001;8(6):315-9.
- Benzel EC, Hart BL, Ball PA et al. Magnetic resonance imaging for the evaluation of patients with occult cervical spine injury. Journal of Neurosurgery 1996;85(5):824-9.
- Como JJ, Diaz JJ, Dunham CM et al. Practice management guidelines for identification of cervical spine injuries following trauma” – update from the Eastern Association for the Surgery of Trauma Practice Management Guidelines Committee 2009.
- Davis JW, Kaups KL, Cunningham MA et al. Routine evaluation of the cervical spine in head-injured patients with dynamic fluroscopy: a reapprasial. Journal of Trauma-Injury Infection & Critical Care 2001;50(6):1044-1047.
- Verhagen AP, Scholtne-Peeters G GGM, Van Wijngaarden S et al. Conservative Treatments of whiplash. Cochrane Database of Systematic Reviews, Issue 4, 2009.
- Côté P, Cassidy JD, Carroll L et al. A Systematic Review of the Prognosis of Acute Whiplash and a New Conceptual Framework to Synthesize the Literature. Spine 2001;26(19):E445-E458.
- NICE, Spinal injury: assessment and initial management; [Guideline: NG41]. Published: 17 February 2016.
- Bandiera G, Stiell IG, Wells GA et al. The Canadian C-spine rule performs better than unstructured physician judgment. Ann Emerg Med 2003;42(3):395-402.
- Rezaie S, Spinal Immobilization in Trauma Patients; Contemporary research links for immobilisation. REBELEM, 2017.























27 Comments
A comprehensive overview of injuries of the cspine
great overview, thanks
Very informative and a helpful revision
nice review of evidence
Good one. Instruction from lawyer is one of the poor prognostic factors
Very good explanation of C-spine injuries. Excellent overview of C-spine injuries.
Great review of c- spine injuries
Enjoyed the read.
Useful information. Really been nice addition to my knowledge.
Great comprehensive review
great
Thank you. Really informative module
effectice reminders
An excellent resource and a cheat sheet for teachings!!
very use full,did find the explanation of the CSR and Nexus and rationale of its application very help fun
GOOD material
Good insight into c-spine injury. Will use this in practice.
Very informative. Would recommend to colleagues.
Thank you
great module.
Very helpful
Highly informative
All about C spine. Good stuff
useful approach guide.
very nice module
Clear concise and excellent.
Thank you , useful information