Author: Jason Lee / Editor: Jason Kendall / Reviewer: Jon Bailey, Kathryn Blackmore / Codes: IP1, ResC7, ResP2, ResP4, RP5, RP6, SLO1, SLO3 / Published: 21/11/2022
Context
This session focuses on community acquired pneumonia (CAP), which is by far the commonest form of pneumonia seen in the emergency department (ED).
Many countries have developed national guidelines for the treatment of CAP. The British Thoracic Society (BTS) guidelines, updated in 2009, and the National Institute for Health and Care Excellence (NICE) guidelines updated in 2014, form the basis for the recommendations made in this session [1,2,3,4]. These guidelines are not applicable to the following patients:
- Children
- Patients with COPD
- Immunosuppressed patients, inpatients
- Patients that have left hospital in the preceding 10 days
Every year between 0.5% and 1% of adults in the UK will have community-acquired pneumonia. It is diagnosed in 5-12% of adults who present to GPs with symptoms of lower respiratory tract infection, and 22-42% of these are admitted to hospital, where the mortality rate is between 5% and 14%. Between 1.2% and 10% of adults admitted to hospital with community-acquired pneumonia are managed in an intensive care unit, and for these patients the risk of dying is more than 30%. More than half of pneumonia-related deaths occur in people older than 84 years.
Mortality for patients with CAP treated in the community is very low (<1%) but is greater than 5% for patients requiring hospital admission, and greater than 30% for patients requiring intensive care input.
Pneumonia remains one of the commonest causes of in-hospital death and carries a significant burden of cost to the UK health system, mainly due to the cost of inpatient care. In 1993, this cost was estimated at 441 million [5]. Hospital admissions for pneumonia rose by 34% between 1997 and 2005 and today the annual cost may exceed 1billion.
History
Although a confident diagnosis of pneumonia cannot be made on the basis of history alone it is unlikely that the patient with none of the following symptoms will have pneumonia.
- Fever
- Productive cough
- Sweating
- Shivering
- Myalgia
- Dyspnoea
- Pleuritic chest pain
The history should also identify factors which may influence the management plan if a diagnosis of pneumonia is made.
These would include the following:
- Prior or current antibiotic use
- Allergies
- Current medications
- Known respiratory disease eg COPD
- Co-morbidities (eg congestive cardiac failure, chronic renal failure)
- Immunosuppression (through disease, or medication)
- Social circumstances
- Smoker
- Age >50 years
- New confusion reported by friend, relative or carer
Only 20% of UK cases of Chlamydia psittaci pneumonia have a history of bird contact, less than 10% of cases of Coxiella burnetii have a history of occupational exposure to animal sources (usually sheep) and less than a quarter of legionella cases occur in clusters. The low frequency of CAP caused by atypical pathogens coupled with the likely high prevalence of the relevant risk factors in the general population means that routine enquiry about such factors is likely to be misleading . Only in those with severe illness, where the frequency of legionella and staphylococcal infection is higher, does the BTS consider questioning about foreign travel and influenza symptoms to be of predictive value.
Organism specific features
Whilst the BTS community acquired pneumonia guidelines acknowledge that certain features occur more frequently with particular organisms (see below), they consider none to be specific enough to influence the initial choice of antibiotic.
Streptococcus pneumoniae
- Increasing age, co-morbidity, acute onset, high fever and pleuritic chest pain
Legionella pneumophila
- Younger patients, smokers, absence of co-morbidity, diarrhoea, neurological symptoms, more severe infection, evidence of multisystem involvement (e.g. abnormal liver function tests, elevated serum creatinine kinase). Legionella infection peaks in autumn in the UK and in 50% of cases is related to travel abroad. Less frequently cases occurs in clusters due to contaminated water cooling systems.
Mycoplasma pneumoniae
- Younger patients, less multisystem involvement. Epidemics occur in UK spanning 3 winters every 4 years.
Staphylococcus aureus
- Incidence peaks in winter and occurs more commonly in intravenous drug users or debilitated patients, particularly those with influenza. It is relatively more prevalent in patients on intensive care but even in this setting strep. pneumoniae remains the most common cause of pneumonia.
Learning Bite
Whilst certain features occur more frequently with particular organisms none are specific enough to influence the initial choice of antibiotic.
Examination
A thorough examination of the cardio-respiratory system should be made to identify features consistent with pneumonia eg bronchial breathing, dullness to percussion, crepitations on auscultation of the chest, pyrexia, tachypnoea and tachycardia. Alternatively, the findings on chest examination may point to an alternative diagnosis such as pulmonary oedema, pleural effusion or pneumothorax.
As a minimum the following parameters should be recorded:
- Temperature
- Blood pressure
- Pulse
- Respiratory rate
- Oxygen saturations
Dependent on the predominant presenting symptom the examination should also focus on areas (e.g. throat, legs) that may reveal features consistent with an alternative diagnosis (e.g. URTI, DVT/PE).
Radiology
CT chest
CT has no role in the routine investigation of patients with CAP.
Chest radiograph
The chest radiograph is the single most useful test available in the ED for diagnosing pneumonia. It is also useful in the identification of alternative diagnoses such as pulmonary oedema and exclusion of others e.g. pneumothorax. The BTS guidelines1 recommend that chest radiographs are performed on all patients being admitted from the ED with CAP in order to confirm or refute the diagnosis.
Chest radiographs are not necessary on patients discharged from the ED with a diagnosis of CAP unless the diagnosis is in doubt or the patient is considered at risk of underlying pathology such as lung cancer.
Chest radiograph changes consistent with pneumonia
The lung parenchymal inflammation and fluid filled alveoli are seen as areas of consolidation on the chest radiograph. The areas of infection are usually limited by pleural surfaces to a specific lobe of one lung but occasionally it may involve more than one lobe or both lungs. Small pleural effusions are common and usually reactive. Occasionally, chest radiographs may appear normal in the early stages of pneumonia. AP films performed on very unwell in the resuscitation room are often of poor quality and distinguishing between pulmonary oedema and pneumonia can be difficult. The following signs may help to confirm a diagnosis of pneumonia:
Silhouette sign:
The silhouette sign refers to the loss of the normal border between structures e.g.
- middle lobe pneumonia, where the right heart margin is classically lost
- right lower lobe pneumonia, where the border of the diaphragm on the right side is obscured, while the right heart margin remains clear
Air bronchogram:
As the bronchi branch a point is reached where the cartilaginous bronchial walls are too thin to visualise (unless calcified) and it is not possible to distinguish air in the bronchi from air in the surrounding alveoli. However, if the surrounding alveoli fill with fluid or pus then branching radiolucent air passages (air bronchograms) may be seen.
Learning Bite
Left lower lobe pneumonia may be missed if the area behind the cardiac shadow is not routinely inspected.
Blood tests
The BTS guidelines recommend that the following tests be performed on all patients admitted with CAP:
Full Blood count
A white cell count >15 x 109/l is suggestive of a bacterial pneumonia.
Urea and electrolytes
Urea forms part of the CURB-65 scoring system. Occasionally, patients will be identified with unsuspected renal failure or hyponatraemia.
C- Reactive Protein (CRP)
CRP levels on admission have not proven to be clinically useful either diagnostically or prognostically but forms a baseline for later comparison. Failure of the CRP level to fall 72 hours after admission suggests treatment failure.
Liver Function Tests (LFTs)
The value of routine measurement of LFTs in patients that are not jaundiced, with non-severe pneumonia is unclear.
Arterial Blood Gases/Lactate
The BTS guidelines recommend that ABGs only be performed in patients with oxygen saturations below 94%3. However, the measuring of lactate levels (which is now routinely measured on most blood gas analysers) is essential for identifying tissue hypo-perfusion in patients who are not yet hypotensive but who are at risk for septic shock. A raised lactate (particularly levels >4mmol/l) is a poor prognostic indicator independent of the CURD-65 score. Early goal directed therapy using sepsis bundle pathways on intensive care have been shown to increase the chance of survival for patients with severe sepsis [11,12].
Microbiology Blood cultures
Overall, blood cultures have a low sensitivity in CAP (<10% cases). The yield is particularly low for patients with non-severe CAP and no co-morbid disease, and for those who have received antibiotic therapy prior to admission [7,8].
The BTS guidelines recommend that blood cultures are taken from all patients with moderate or severe CAP and most other patients admitted with CAP, preferably before antibiotic therapy is commenced.
However, blood cultures may be omitted if the following criteria are met-
- a diagnosis of CAP has been definitely confirmed
and
- the patient has low severity pneumonia
and
- the patient has no significant co-morbid disease
Learning Bite
Blood cultures are not required for patients with confirmed low severity pneumonia in the absence of co-morbid conditions.
Microbiology Sputum culture
Purulent sputum samples should be sent for culture and sensitivity from patients with the following characteristics[1]:-
- Severe pneumonia
- Moderate pneumonia that have not received prior antibiotics
- Failure to improve with treatment
- Patients who test positive for urine legionella antigen
Since the aim is to deliver antibiotics within 4 hours of arrival at the ED, purulent sputum samples that are produced by patients being admitted with CAP should in general be sent for culture and sensitivity. Samples obtained later on the ward will have a lower yield due to antibiotic administration in the ED.
Serology
A number of serological tests are available for identification of specific organisms but are of little relevance to management of the patient in the ED.
The BTS guidelines recommend the following:
Pneumococcal urine antigen
All patients with moderate or severe CAP should be tested.
Legionella urine antigen
Patients with severe pneumonia, specific risk factors and all patients during epidemics should be tested. NICE recommends testing patients with moderate or severe pneumonia.
PCR
PCR testing is available for mycoplasma pneumonia, Chlamydophila and respiratory viruses but should be selectively requested by respiratory physicians.
ECG
Pneumonia is not associated with specific ECG changes though sinus tachycardias are common. In the elderly it is not uncommon for pneumonia to trigger atrial fibrillation or rate related ischaemia.
Risk stratification
The CURB-65 score is made up from the following components (1 point for each):
- Confusion (new onset disorientation in time, place or person) OR an AMT score of (< 8/10)
- Urea: > 7mmol/l
- Respiratory rate: > 30/min
- Blood pressure: low blood pressure (systolic BP < 90 mm Hg or diastolic BP < 60 mm Hg)
- Age: >65 years
Abbreviated Mental Test (AMT) score
Patients with new confusion (disorientation in time, place or person) secondary to pneumonia are stratified by the CURB-65 system into a higher mortality risk group than those that are not confused. It is not uncommon to meet confused patients in the ED that have been brought by ambulance from care homes and be unsure whether their confusion is old or new. In this situation a score of 8 or less on the AMT is substituted for confusion in the CURB-65 score.

Learning Bite
Confusion (new onset disorientation in time, place or person) OR an AMT score of ( 8/10) scores 1 point on the CURB-65 score
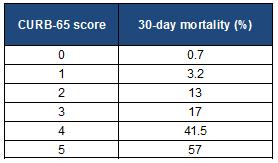
CURB-65
The possible score ranges from 0-5 and the mortality from pneumonia rises exponentially with the CURB-65 score as seen in the table below [10].
The BTS adopted this scoring system in 2004 as it is easy to use (being a single step system compared to previous multi-step systems) and it is clinically useful in determining the disposition of patients. The BTS classifies patients scoring 3 or more are as having severe pneumonia and recommends that these patients are admitted urgently. Hospital treatment should be considered for those scoring 2 but outpatient management is acceptable in selected cases. Most patients with CAP who have CURB-65 scores of 0 or 1 can be managed in the community.
Learning Bite
A CURB-65 score of 3 or more indicates a severe pneumonia.
Other factors suggesting a need for admission
The vast majority of patients with a CURB-65 score of 0 or 1 can be discharged. However, the BTS considers additional factors that are adversely related to prognosis to be important in deciding whether patients require in-patient treatment or not, irrespective of their CURB-65 score. These include:
-
- Hypoxaemia (SaO2 <94% or PaO2 <8 kPa)
- Bilateral or multi-lobe involvement on the chest radiograph
- Presence of a co-existing disease e.g. Congestive cardiac failure, chronic renal failure
- Age over 50 years
Some elderly patients with no adverse factors (other than age) will require admission solely for social reasons.
Learning Bite
The CURB-65 score should not be used in isolation to risk stratify patients.
General management
Patients should be given the following advice(1):
- rest
- drink plenty of fluids
- stop smoking
Patients discharged from the ED should be advised to see their GP for review within 48 hours or sooner if clinically indicated.
Specific management
Antibiotics
Local guidelines should be adhered to but listed below are pragmatic antibiotic regimes that the BTS support.
Patients with low severity pneumonia that are either discharged or admitted (for social reasons or because of significant co-morbidities) and most with moderate severity pneumonia should be prescribed oral antibiotics if they are able to swallow:
- Amoxicillin 500mg orally, three times per day for 1 week is the preferred regime.
- Clarithromycin 500mg orally, twice per day for one week is an alternative if the patient is allergic to penicillin.
- Levofloxacin 500mg orally once daily can be used for patients allergic to both drugs mentioned above.
Admitted patients with low and moderate severity pneumonia that are unable to swallow should be given intravenous antibiotics.
Admitted patients with severe pneumonia should be given intravenous antibiotics as soon as possible after the diagnosis made.
The BTS guidelines recommend Co-amoxiclav 1.2 g IV TDS plus Clarithromycin 500 mg IV BD for 7-10 days as an appropriate first-line treatment. However, local resistance patterns and other factors may mean that some hospitals recommend alternative first-line therapy. In this situation local guidelines should be followed.
If penicillin allergic, consider Cefuroxime plus Clarithromycin. If penicillin and clarithromycin allergic, consider Levofloxacin.
Learning Bite
Antibiotics should be started in the ED as soon as possible after the diagnosis is made (usually on chest radiography) and within 4 hours of arrival in all cases. Local antibiotic guidelines should be followed.
Oxygen
The BTS oxygen guidelines [6] should be followed. Oxygen should be prescribed and administered if the oxygen saturations are below 94% on air or the arterial oxygen tension PaO2 is less than 8kPa.
Steroids
Steroids are not recommended in the routine treatment of pneumonia of any severity.
Chest physiotherapy
Classical chest clearance techniques are not routinely recommended for patients admitted with pneumonia but may have a place in patients with pre-existing lung conditions.
NIV
CPAP and NIV have not been demonstrated to improve mortality in patients with respiratory failure secondary to pneumonia and their routine use is not recommended.
Para-pneumonic effusions
Para-pneumonic effusions are found in up to a half of all patients admitted with CAP. Thoracocentesis is recommended in all cases to identify those that are infected (empyemas).
Where there is evidence that the pleural aspirate is infected (clear but pH<7.2 or cloudy /pus) a pleural drain should be inserted.
Follow up
A letter should be sent to the GP recommending that a chest radiograph be repeated 6 weeks after completion of treatment for the following patient groups:
- Persistence of symptoms or signs.
- Patients at higher risk of malignancy (especially smokers and those aged over 50 years).
Potential pitfalls include:
- Applying CAP guidelines to children, immunosuppressed patients or patients with COPD.
- Decision making based on the CURB-65 score alone.
- Prescribing intravenous antibiotics for all patients.
- Failure to send sputum samples before antibiotics are administered.
- Failure to recognise the patient with sepsis.
- Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, Macfarlane JT, Read RC, Roberts HJ, Levy ML, Wani M, Woodhead MA; Pneumonia Guidelines Committee of the BTS Standards of Care Committee. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009 Oct;64 Suppl 3:iii1-55. doi: 10.1136/thx.2009.121434.
- National Institute for Health and Care Excellence. Pneumonia in adults: diagnosis and management. NICE [CG191] Last updated: 07 July 2022.
- British Thoracic Society. Annotated BTS Guideline for the management of CAP in adults. Summary of recommendations (2015).
- Lim WS, Smith DL, Wise MP, Welham SA; British Thoracic Society. British Thoracic Society community acquired pneumonia guideline and the NICE pneumonia guideline: how they fit together. Thorax. 2015 Jul;70(7):698-700.
- Guest JF, Morris A. Community-acquired pneumonia: the annual cost to the National Health Service in the UK. Eur Respir J. 1997 Jul;10(7):1530-4.
- O’Driscoll BR, Howard LS, Davison AG. BTS guideline for emergency oxygen use in adult patients. Thorax 2008;63:vi1-vi68.
- Campbell SG, Marrie TJ, et al. Utility of blood cultures in the management of adults with community acquired pneumonia discharged from the emergency department. Emerg Med J. 2003;20(6):521-523
- Campbell SG, Marrie TJ, et al. The contribution of blood cultures to the clinical management of adult patients admitted to the hospital with community-acquired pneumonia: a prospective observational study. Chest. 2003;123(4):1142-1150.
- Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing. 1972 Nov;1(4):233-8. doi: 10.1093/ageing/1.4.233..
- Lim WS, van der Eerden MM, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003 May;58(5):377-82.
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M; Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001 Nov 8;345(19):1368-77.
- Shapiro NI, Howell MD, Talmor D, et al. Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med. 2005 May;45(5):524-8.




7 Comments
Very thorough summary of CAP with helpful learning bites and pitfalls
very useful topic
Thorough and useful.
Very useful information about CAP
Very useful and concise. Thank you.
Thank you. Very informative
Very well constructed, thank you