Author: Nikki Abela / Editors: Charlotte Davies, Elizabeth Herrieven / Codes: SaC1, SaC2, SaP2, SLO12, SLO5, SLO7, SLO8 / Published: 12/09/2018
The dark side of PEM, and what should also be on your differential diagnosis for any patient you are seeing is: “was this inflicted” and “is there something more?”.
Child abuse is unfortunately something that happens and as doctors we play a crucial role in safeguarding patients from it. You may be the only person who has the single opportunity to do this. Don’t dismiss any nagging feeling if you think something isn’t quite right: find a friend (senior colleague or nurse) and discuss your concerns.
An abused child who is returned to an unsafe home environment is at 50 percent risk for further injury and 10 percent risk of death over the next five years. You can not afford to let this slide.
Early identification of, and intervention in, households where children have been abused can lower the recurrence rate to less than 10 per cent.
Child abuse comes in many shapes and forms: physical, emotional and sexual abuse, neglect or other exploitation.
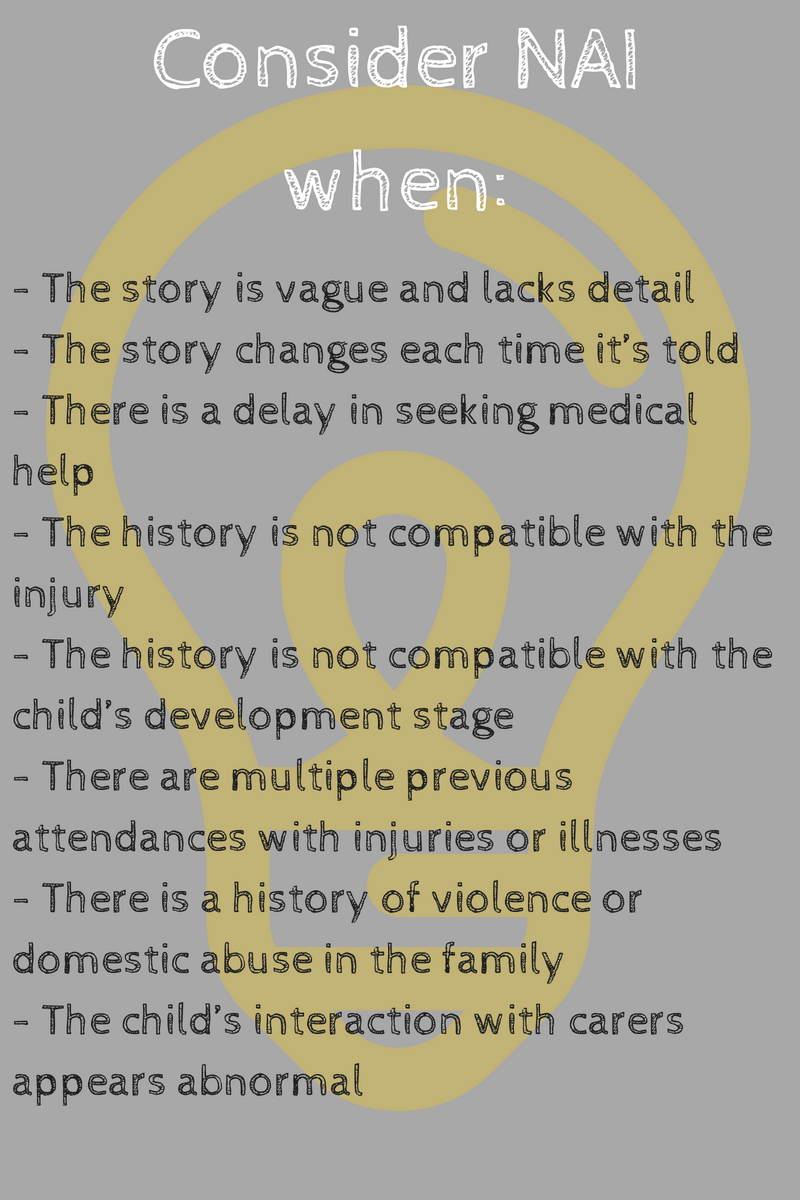
We should be all ears in the history to think of inconsistent findings and most departments will have a checklist of red flags for abuse which will look something like this:
Physical abuse takes many forms: burns are the most common, followed by fractures and bruises.
When examining the child pay particular attention to:
- Injuries that don’t fit the history
- Multiple fractures in various stages of healing, or different types of injuries
- Injuries that are likely to be inflicted
- Evidence of poor caretaking
- Sudden onset of altered mental status not attributable to medical illness
- Any bruising in a child that is not yet cruising
- Bruising to the pinna, neck, or abdomen
- Injury to the genitalia
You can think of these as the 6 Bs – Bruises, Breaks, Bonks, Burns, Bites, Baby blues. Looking further at bruises, it is common for children to have many bruises, especially over bony surfaces like shins and chins. However, these bruises should make you think of non-accidental injury:
- Buttocks, trunk, genitals, ears and back of hands.
- Bilateral, symmetrical or geometric
- Bruise resembles shape of an instrument (e.g. belt buckle, hand knuckles, spoon)
- Multiple bruises of various colours on the same area
If you like these mnemonics, you can think of these as the TEN-4 FACES Bruising Rule.
Remember:
Children who can’t cruise shouldn’t bruise
Burns can also be accidental, but 15-25% are thought to be the result of abuse, so pay particular attention to patterns that mimic objects, especially hot plates, hair straightening irons, steam irons, cigarettes etc. Remember that although children do like to explore, they wont touch a hot object for long.
Immersion burns on buttocks, hands or feet can occur if the child is lowered into hot water accidentally or non-accidentally. Look out for the absence of splashes, which indicates the child was unable to thrash around.
Fractures are the second most common manifestation of abuse after burns, and you should really be able to match the fracture pattern with the reported mechanism of injury. If it doesn’t make sense, don’t be afraid to go back and clarify the fine details. Any fracture can be caused by abuse, so it is all about piecing the puzzle together. If the history keeps changing, then start to worry.
Remember, that the very young are non-ambulatory, so there are very few plausible ways for them to sustain injuries. They are particularly at risk because the are non-verbal.
You need to think about NAI in any non-verbal child who presents with a low GCS: the classic triad of retinal haemorrhages, subdural haemorrhage and rib fractures is what diagnoses the abuse, but in the ED you will only have a small piece of the puzzle (the child with signs or symptoms of a head injury) and it is up to you to find the other pieces and form the picture.
Sexual abuse may manifest in many ways. Children may say they have been raped, but commonly signs are more subtle and you have to look for them. Things like STIs, excessive sexual knowledge or genital trauma are generally things you need to search for, so do look if the context necessitates. In teenagers you should really be on the lookout for child sexual exploitation, and in young girls and boys of the right age, make it routine practise to ask about their relationships, with whom and how old are they and whether they are sexually active.
Emotional abuse occurs when an adult harms a child’s development by repeatedly treating and speaking to a child in ways that damage the child’s ability to feel and express their feelings. Signs include:
- Parent or guardian constantly criticizing the child
- Child shows extremes of behaviour and displays anxiety
- Delayed physical, emotional, or intellectual development
- Compulsive lying and stealing
- Displays feelings of worthlessness
- Eating hungrily or hardly at all
- Attention seeking
- Reluctance to go home
- Fearfulness when approached by a person known to them
Neglect is the commonest form of abuse reported to services. According to the NSPCC, one in 6 (16%) young adults were neglected at some point during childhood with one in 10 young adults (9%) severely neglected during childhood.
It encompasses both actual and potential harm and may be picked up when a child is brought to the ED. Sometimes it may be obvious, but other times it may become evident on taking a detailed history.
Look at the child in front of you as a whole being, not just the simple (and likely accidental) injury they may have been brought in for. Are their clothes inappropriately soiled? Did anyone other than a parent bring them in and why? Are the parents supportive about the interventions you are doing?
Remember also the child is part of a family unit which may be under a lot of strain, but do look out for inappropriate interaction between parents (if their relationship is abusive than the child is at risk too), and also compare them to siblings who may accompany them.
On a final note, don’t go pointing any fingers in the emergency department, but be honest and open with parents about investigation (except in Munchausen syndrome by proxy, but that is another topic). Remember things may not always be what they initially seem, and other causes need excluding!
Further Reading
Long Bone Fracture and NAI
Recognition of Child Abuse podcast
Paediatric Physical Abuse
Page 14: RCEM Safeguarding Standards
Safeguarding e-learning on elfh




4 Comments
Very helpful summary with useful links too
very valueble.thanks
Good update on safeguarding in ED
Good refresher