Author: Victoria L Henson / Editor: Jason M Kendall / Reviewer: Louise Burrows, Peter Kilgour / Code: ACCS LO 2, CC4, CP1, CP2, ResC6, ResP2, RP5, SLO1, SLO3 / Published: 22/03/2021
Cardiogenic pulmonary oedema (CPO) is a common presentation to the Emergency Department (ED).
There are 3 key issues in the management of CPO:
- correct and early identification of the condition
- prompt instigation of appropriate treatment
- detection of the underlying cause.
Patients who present with CPO have a poor long term outcome but their short term mortality can be improved by early correct management.
There is no formal definition of CPO; however it is characterised by the presence of excess fluid within the pulmonary interstitium and, at its most severe, within the alveoli. CPO is pulmonary oedema due to a primary cardiac or circulatory cause rather than other forms of pulmonary oedema (eg. neurogenic pulmonary oedema). CPO may be a feature of several different types of acute heart failure presentation (see Figure 1).
Figure 1: Clinical Presentations of Acute Heart Failure
The European Society of Cardiologys (ESC) 2016 Guidelines on heart failure defined heart failure as patients with all of the following(1):
- Symptoms typical of heart failure
- Signs of heart failure
- Objective evidence of structural or functional abnormality of the heart at rest
The ESC Guidelines defined acute heart failure as:
A rapid onset or change in signs or symptoms of heart failure, resulting in the need for urgent therapy . Patients may present as a medical emergency such as acute pulmonary oedema.(1)
Pathophysiology
CPO arises due to a combination of problems arising within the circulatory system which have a knock on effect on one another causing a spiralling cycle of increasing fluid accumulation within the lungs which hinders gas exchange leading to worsening hypoxia and respiratory failure (see Figure 2).
Figure 2: Pathophysiology of CPO
If the left ventricle is unable to empty the blood that it receives from the lungs, there is a consequent rise in the end diastolic volume and pressure. This causes the normally low pressure system of the pulmonary vasculature to increase resulting in hydrostatic pressure exceeding oncotic pressure. Fluid then transudates into the interstitium and the alveoli; once this leak exceeds the lymphatics ability to reabsorb fluid the accumulating fluid hinders gas exchange and hypoxia develops.
Hypoxia triggers catecholamine release which causes vasoconstriction and subsequent increased systemic vascular resistance, which further impedes the ability of the left ventricle to empty. The renin-angiotensin-aldosterone system is activated leading to salt and water retention, an increase in sympathetic tone and a subsequent increase in both afterload and preload. The escalation in both oxygen demand and consumption due to the increases in cardiac and respiratory work load are unable to be met as gas exchange within the lung fails and tissue hypoxia ensues.
Although there are multiple precipitating causes of CPO (see Figure 3) there appears to be clinically two main groups. Those with (i) pump failure ie. systolic dysfunction with a reduced ejection fraction and (ii) those with diastolic dysfunction and preserved ejection fraction. This latter group are often hypertensive and have stiff left ventricles which are unable to relax.
Figure 3: Precipitating Causes of Acute Heart Failure
Patients with CPO classically present to the ED in extremis, often in the early morning. The history is often limited initially and CPO can prove to be a difficult diagnosis to make, as it frequently occurs in patients with coexisting COPD and those at risk of pneumonia or pulmonary embolism. Rapidly establishing the diagnosis and identifying any precipitating causes will allow instigation of appropriate treatment, alleviation of the patients distressing symptoms and improvement in their outcome.
(i) History
The history should focus on establishing the diagnosis of CPO as well identifying any precipitating event. Previous episodes of CPO, orthopnoea or PND together with any historical factors that could point towards a precipitating cause should be elicited (see Figure 3).
Table 1 lists typical historical features of patients presenting with respiratory distress to help distinguish CPO from other causes.
Table 1: Features in the history which help to distinguish CPO from other pathologies
| Symptom | CPO | COPD | Pneumonia | PE | Precipitating Cause e.g. ACS |
| SOB | ++ | + | + | + | |
| Cough | + pink frothy sputum |
+ Dry cough |
+ Green sputum |
+ Haemoptysis |
|
| Chest pain | + | + | + | ||
| Palpitations | + | + | + | ++ | |
| Fever | + | ++ | |||
| Sweating | ++ | + | + | + | |
| Acuity | + | + | + | ||
| Nocturnal | ++ |
(ii) Clinical examination (see Box 1 and Table 2)
Box 1: Typical examination findings in a patient with acute pulmonary oedema
Airway
- Usually intact, unless conscious level impaired by hypoxia or hypercapnoea.
- In extreme cases blood stained frothy sputum may be present
Breathing
- Tachypnoea is typical and the patient may be fighting for breath, using accessory muscles and adapting their posture to maximise air entry.
- The bases may be dull to percussion as small pleural effusions are common particularly in acutely decompensated chronic heart failure
- O2 saturations are typically <90% on air
- Auscultation reveals bibasal inspiratory crepitations which extend higher up the chest as the condition worsens. In some cases wheeze predominates which can confuse the picture.
Circulation
- Patients appear diaphoretic pale and their skin cold and clammy
- Monitoring stickers and line adhesive may not stick as the patient sweats profusely.
- Sinus tachycardia is common but arrhythmias such as new atrial fibrillation may precipitate CPO.
- The blood pressure is usually high; however, hypotension may be present and is associated with cardiogenic shock and increased mortality.
- The heart sounds may be inaudible over the rales from the lungs but a gallop rhythm may be present. Murmurs, especially mitral regurgitation and aortic stenosis, should be listened for, and may reveal a precipitating cause.
- Level of hydration should be assessed. Some patients may be fluid overloaded but many are euvovolaemic. Assess the JVP, mucus membranes and urine output. Look for peripheral oedema and hepatomegaly suggesting right heart failure.
Disability
Initially patients are alert and anxious. As their hypoxia worsens they may become agitated and with worsening respiratory failure may become hypercapnoeic causing their conscious level to fall.
Exposure
Afebrile with cold and clammy skin
Table 2: Typical clinical features and differential diagnosis of CPO
| Sign | CPO | COPD | Pneumonia | PE |
| Heart rate | ↑↑ | ↑ | ↑↑ | ↑↑ |
| Blood pressure | ↑ | → | ↓ | ↓ |
| Temperature | → | → | ↑ | → |
| O2 saturations | ↓↓ | ↓ | ↓ | ↓ |
| Chest signs | Bilateral crepitations | Diffuse wheeze | Focal crepitations | Clear
|
| Skin | Cold, pale and clammy | Dry and warm | Flushed and warm | Dry |
| Heart sounds | Murmurs, 3rd/4th heart sounds | Normal | Normal | Normal |
The combination of history and examination will often lead to the appropriate diagnosis. However, the following investigations will confirm the suspected diagnosis and enable evaluation of the severity of the clinical situation.
Box 2: Essential initial investigations in the Emergency Department
ECG (see figures 4, 5 and 6):
- The ECG is rarely entirely normal in patients with CPO, although there are no diagnostic features specific to CPO.
- It will often show a tachycardia and possible left ventricular hypertrophy.
- It may reveal precipitating causes such as ST segment changes associated with an ACS (STEMI or NSTEMI) or an arrhythmia eg atrial fibrillation.
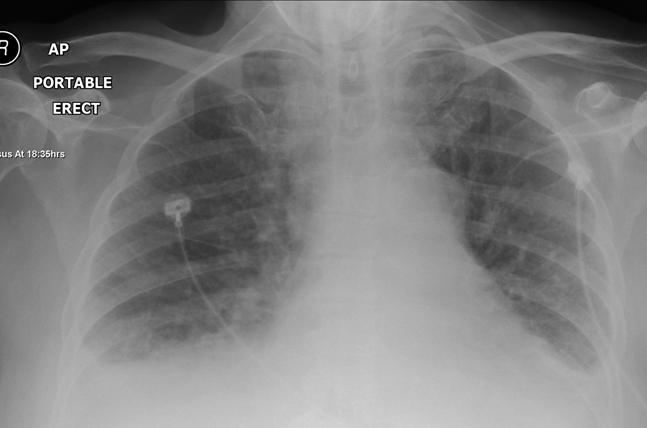
CXR (see figures 7 and 8):
- The CXR is usually helpful in excluding other causes of breathlessness, such as pneumonia or pneumothorax.
- A normal CXR in the acutely short of breath patient would be more likely to suggest a pulmonary embolus or COPD/asthma.
- Typical radiological findings are demonstrated in figures 7 and 8. They include pleural effusions, cardiogmegaly, interstitial and alveolar oedema and upper lobe diversion.
Arterial Blood Gas (see Boxes 3 and 4):
- Hypoxaemia is the commonest finding and is often out of proportion to the level of hypercapnoea. (ie Type 1 respiratory failure); this contrasts with COPD patients in extremis (who have type 2 respiratory failure).
- In pre-existing chronic lung disease or impaired conscious level hypercapnoea and hypoxia may develop. (ie Type 2 respiratory failure)
- Acid base balance and lactate will aid assessment of tissue perfusion.
Venous Blood Tests:
- Baseline bloods including FBC, U&Es, LFT, and INR should be taken.
- Infection, renal or liver failure, anaemia or electrolyte abnormalities can be identified which may precipitate or exacerbate CPO.
- Hyponatraemia and raised urea and creatinine are associated with poor outcome.
- Troponin should be measured and may support an ACS diagnosis (which is associated with an adverse outcome) but small rises in Troponin can occur in CPO without ACS.
Fig 4: Example ECG 1 in CPO Sinus Tachycardia with widespread T wave inversion and Q waves V1 and V2
Fig 5: Example ECG 2 in CPO Atrial flutter with 2:1 block

Fig 6: Example ECG 3 Atrial fibrillation with ventricular ectopics and lateral T wave inversion
Fig 7: CXR Large heart and interstitial and alveolar oedema
Fig 8: CXR Bilateral pleural effusions and upper lobe diversion
Box 3: Typical CPO ABG on air:
Type 1 respiratory failure with hypoxia and a metabolic acidosis
| pH | 7.29 |
| pCO2 | 4.92 |
| pO2 | 6.80 |
| Sats | 84% |
| HCO3 | 16 |
| BXS | -5 |
| Lactate | 3.2 mmol/L |
Box 4: ABG in Advanced CPO with co-existent COPD on 15L% O2:
Type 2 respiratory failure with relative hypoxia and a mixed respiratory and metabolic acidosis
| pH | 7.12 |
| pCO2 | 8.5 |
| pO2 | 12.3 |
| Sats | 92% |
| HCO3 | 13 |
| BXS | -6 |
| Lactate | 5.8 mmol/L |
(i) Echocardiography:
This may not be available within the Emergency Department but it should be performed during the admission. If a mechanical problem is suspected such as valve dysfunction, ventricular wall rupture or tamponade, urgent echocardiography should be arranged.
(ii) B Type Natriuretic Peptide (BNP):
BNP is produced by cardiac myocytes in response to stretch which occurs in impaired diastolic or systolic function. BNP may play an important role in acute cardiac failure. BNP assays can supplement clinical judgment when the cause of a patient’s dyspnoea is uncertain. Results should be interpreted in the context of all available clinical data. The role of BNP in chronic heart failure is, however, well established for diagnosing, staging and risk stratifying patients. [9]
BNP has reasonable sensitivity and therefore can be used to rule out heart failure as a cause of a patients breathlessness (in a primary care setting for example) but it is not very specific and therefore not useful for ruling the diagnosis in. BNP rises due to sepsis, renal or liver failure, hypoxia, myocardial ischaemia, tachycardia as well as many other reasons. In hyperacute or flash pulmonary oedema or acute mitral regurgitation the BNP level may not be elevated initially.
The priorities are to relieve symptoms and to restore haemodynamic stability and tissue perfusion. The approach to management is summarised in Box 5.
Box 5: Emergency Management of CPO:
| Airway | Positioning |
| Breathing | High flow O2 CPAP/BiPAP |
| Circulation | Nitrates Furosemide |
| Disability | Morphine |
| Exposure | Positioning |
(a) Airway
Allow the patient to find the best position for their airway and breathing. If the airway is compromised intervene as required. This may be due to (i) a reduction in conscious level due to hypoxia, hypercapnoea or excessive opiate administration, or (ii) due to pulmonary oedema fluid exuding from the lungs.
(b) Breathing
- British Thoracic Society Guidelines suggest in acute heart failure, aim for an oxygen saturation of 94-98% [2].
- High flow O2: 15L/minute with a reservoir bag is required for most patients, as hypoxia is frequently the key problem.
- Patients with coexistent COPD or otherwise at risk of hypercapnia need careful monitoring. When feasible the inspired O2 can be reduced to achieve target saturations of 88-92%.
- Once non-invasive ventilation (NIV) is initiated, O2 supplementation will still be required
(i) Oxygen
- High flow O2: 15L/minute with a reservoir bag is required for most patients (unless known to retain CO2), as hypoxia is frequently the key problem.
- British Thoracic Society Guidelines suggest supplemental O2 is required only if saturations are < 95% and the patient is short of breath(2).
- Patients with coexistent COPD need careful monitoring. When feasible the inspired O2 can be reduced to achieve saturations of 90-92%.
- Once non-invasive ventilation (NIV) is initiated O2 supplementation will still be required.
(ii) Non-invasive Ventilation (NIV)
The aim of NIV is to improve oxygenation, decrease the work of breathing and increase cardiac output. Continuous Positive Airways Pressure (CPAP) provides a constant level of positive airways pressure preventing alveolar collapse. Bi-level Positive Airways Pressure (BiPAP) enables increased CO2 clearance by providing a higher level of positive pressure on inspiration.
Box 6: Evidence Base for Non-invasive ventilation in CPO
A Cochrane Review (2008) systematically reviewed the research data published prior to 2005 and concluded that NIV should be considered and implemented in all CPO patients early unless contraindicated. The Review reported that: (i) CPAP decreased intubations, mortality and length of ITU stay and that (ii) BiPAP may be of use in CO2-retaining patients but that more research was required. In order to avoid 1 death, the number needed to treat (NNT) with CPAP was 9 and to avoid 1 intubation the NNT with CPAP was 6(3).
The 3CPO trial also published in 2008 is the largest multicentre RCT which compared standard medical therapy to BiPAP and CPAP(4). This study found no reduction in mortality or intubation rates in either of the NIV groups but patients felt better more quickly. There was no evidence of additional harm.
The ESC recommends that all CPO patients should be considered for NIV early on in their management (unless contraindicated)(1).
Learning Bite
Consider NIV early in the management of all patients with cardiogenic pulmonary oedema, unless contraindicated
Table 3: Practical aspects related to Non-invasive Ventilation in CPO
| Indications |
|
| Cautions |
|
| Contraindications |
|
| How to deliver NIV |
|
| Complications |
|
(c) Circulation
(i) Diuretics:
Loop diuretics reduce preload by preventing sodium chloride reabsorption in the ascending Loop of Henle, which increases fluid excretion. Preload is also reduced by their vasodilatory action. Both of these actions should be beneficial in a patient with CPO and fluid overload.
For decades diuretics have been the accepted mainstay of treatment in CPO despite a lack of randomised controlled trials demonstrating beneficial outcome; there is some evidence suggesting a detrimental effect at high doses(1,5,6,7,8). Specifically, their use may dehydrate the euvolaemic patient and cause hyponatraemia and hypotension. Also, due to their effect on the renin/angiontensin/aldosterone system and stimulation of the sympathetic system, diuretics may increase afterload thereby decreasing stroke volume and cardiac output.
Patients with CPO generally have elevated systemic vascular resistance and reduced renal perfusion and consequently diuretic action may be delayed by up to 1 hour. It is probably only the vasodilatory action of diuretics that is initially beneficial and this can also be achieved with IV nitrates(5).
The ESC Guidelines advocate small intravenous boluses of furosemide at 20-40mg for patients with CPO and symptoms of fluid overload or congestion. In those with CPO already taking chronic diuretic therapy, the initial IV bolus should be at least equivalent to their usual oral dose [1].
Learning Bite
High dose diuretics should be used with caution and only in those with evidence of fluid overload and a history of long term diuretic use
ii) Vasodilators:
These agents have positive physiological effects by off-loading the heart through their venous and/or arteriolar vasodilatory effects causing a reduction in pre-load and/or after-load. Vasodilators should not be used in patients with a systolic blood pressure of less than 90mmHg or in those with aortic stenosis (who are dependent on sufficient preload to force blood across the gradient).
Nitrates
The majority of patients with CPO have a high-end-of-normal blood pressure at presentation and are able to tolerate nitrates. Initially administer sublingual nitrates until intravenous access is established and then commence IV at a rate of 10-20mcg/min, increasing every 3-5 min by 5-10 mcg/min as needed and as BP allows, up to a maximum of 200mcg/min [1].
Nitroprusside
This is an alternative vasodilator which reduces preload and afterload. It is particularly useful in the rare cases of extreme hypertension precipitating CPO (ie. in a hypertensive emergency).
It can precipitously drop the systolic blood pressure but tolerance is not an issue as it is with nitrates.
The ESC 2016 guidelines suggest cautiously commencing an infusion at 0.3 mcg/Kg/min (titrated up to 5 mcg/Kg/min) with invasive blood pressure monitoring (1).
Nesiritide
- This is a recombinant B-type natriuretic peptide with both a diuretic and natriuretic effect, as well as being a venous and arterial vasodilator.
- It is currently used in the USA but has limited licensing in the UK and Europe.(1)
(iii) Inotropes:
Inotropes should be considered if hypotension or signs of end organ hypoperfusion persist despite use of vasodilators/diuretics.
They should be commenced early once the need is recognised and stopped as soon as adequate tissue perfusion is achieved.
Their use is associated with increased mortality, as they increase cardiac oxygen demand and myocardial injury.
Dobutamine is probably the first choice agent. Infusion is commenced at 2-3mcg/kg/min and increased as required.(1)
(d) Disability
Morphine should be given early for patients who are agitated and distressed or complaining of chest pain.
Opiates also provide a potential physiological benefit due to their vasodilatory effects and resultant reduction in pre-load.
Only small boluses of 2.5-5mg are recommended as opiates may cause hypotension and/or respiratory depression.(1)
Exposure
Position the patient sitting upright supported with pillows as appropriate for their conscious level.
Cardiac failure has a very poor long term outcome and the prognosis can be worse than that of many cancers.
The ESC 2008 Guidelines report that acute heart failure associated with cardiogenic shock has an in-hospital mortality ranging from 40-60%. However, in those that present with hypertensive acute heart failure their in-hospital mortality is low(1).
In the 3CPO trial the 7-day mortality was 9.5% for the NIV arms, 9.8% for the standard therapy arm and 9.9% for non-recruited patients. The 30-day mortality was 15.2% in the combined NIV arms and 16.2% in the standard therapy arm(4).
The following features are associated with a worse outcome: (1)
- Advanced Age
- Wide QRS
- Hyponatraemia
- Low Left Ventricular Ejection Fraction
- Hypotension
- Precipitated by ischaemia
- Previous hospitalisation for heart failure
- Marked BNP elevation
- Elevated troponin
Key Learning Points
- CPO most commonly occurs in the elderly and those with ischaemic or valvular heart disease, hypertension and diabetes.
- Clinical presentation is classically the triad of breathlessness, sweating and agitation.
- The examination findings are tachycardia, tachypnoea, hypoxia and bibasal inspiratory crepitations. A gallop rhythm may be present.
- Blood pressure is generally high. A systolic of <90 mmHg is associated with cardiogenic shock and a significantly higher mortality.
- Precipitating causes must be looked for such as cardiac ischaemia or infarction, acute mitral valve regurgitation, arrhythmias or high output states such as sepsis.
- ABG, CXR and ECG are the key initial investigations needed in the ED. Baseline bloods including troponin should also be performed.
- ABG generally show type 1 respiratory failure.
- Echocardiography should be performed during the admission and, if an acute mechanical cardiac problem is suspected, it should be performed urgently (Class I, level of evidence C)
- Treatment should consist of sitting the patient up, administering high flow O2 (Class I, level of evidence C), intravenous nitrates (Class I, level of evidence B) and instituting NIV if appropriate (Class IIa, level of evidence B).
- Low dose furosemide should also be administered; only use higher doses if the patient is fluid overloaded and/or on maintenance diuretic therapy (Class I, level of evidence B)
- In the agitated patient or those with coexistent chest pain small doses of morphine should be titrated. (Class I, level of evidence C)
- Mistaking COPD for CPO or vice versa
- Mistaking pneumonia for CPO and the consequent misuse of vasodilators and diuretics in septic patients
- Failure to identify and treat the precipitating cause of CPO e.g. STEMI
- Inappropriate use of high dose diuretics in patients with CPO who are euvolaemic or hypovolaemic
- 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal (2016) 37, 21292200.
- O’Driscoll BR, Howard LS, Earis J on behalf of the BTS Emergency Oxygen Guideline Development Group, et al British Thoracic Society Guideline for oxygen use in adults in healthcare and emergency settings BMJ Open Respiratory Research 2017;4:e000170. doi: 10.1136/bmjresp-2016-000170.
- F M R Vital, H Saconato, M T Ladeira, A Sen, et al. Noninvasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema (Review). Cochrane Database of Systemic Reviews 2008, Issue 3.Art.No.: CD005351.DOI: 10.1002/14651858.CD005351.pub2.
- A Gray, S Goodacre, D E Newby, M Masson et al. Noninvasive Ventilation in Acute Cardiogenic Pulmonary Edema. The New England Journal of Medicine. July 10 2008. Vol 359, iss 2: pg 142
- A Mattu, J P Martinez, D S Kelly. Modern Management of Cardiogenic Pulmonary Edema. Emergency Medicine Clinics of North America 23(2005) 1105-1125
- D Feldman, D M Menachemi, W T Abraham, R K Wexler. Management strategies for stage D patients with acute heart failure. Clinical Cardiology 31, 7, 297-301 (2008)
- G Cotter, E Metzkor, Z Faigenerg, R Miller, A Simovitz et al. Randomised trial of high dose isosorbide dinitrate plus low dose furosemide versus high dose furosemide plus low dose isosorbide dinitrate in severe pulmonary oedema. The Lancet. Vol 351, February 7th 1998 page389-393.
- M Metra, J R Teerlink, A A Voors, G M Felker, O Milo-Cotter et al. Vasodilators in the treatment of acute heart failure: what we know, what we dont. Heart failure Reviews. DOI 10.1007/s10741-008-9127-5
- Weintraub NL et al. Acute Heart Failure Syndromes: Emergency Department Presentation, Treatment, and Disposition: Current Approaches and Future Aims. A Scientific Statement From the American Heart Association. Circulation. 2010;122:1975-1996.










24 Comments
Very good overview, please update and keep us informed especially in Ae settings ! thanks!
very good review!!
very good wrap up
Very good review from an ED perspective. An area that often causes conflict with cardiology.
Very useful review
Great summary, would be nice to have this as a learning module too
Thanks for your feedback. You can find a learning session on the same topic here.
comprehensive review
Great Review. Thank you.
Good resource
Good overview
Very useful
Very good material. Thank you.
This material hits the core points.
Clear and concise. Well structured.
Good resource. Very helpful
One of the best session
Great review of the topic
EXCELLENT OVERVIEW OF CPO
Really helpful. Thank you.
This is awesome.
CPO made simple.
All ED doctors need to read this.
Great learning
Useful
excellent