Author: Elizabeth Docherty, Francis P Morris / Editor: Jason Kendall, Chris Gray / Reviewer: Chris Gray, Joshua Davison / Codes: CC3, CP1, CP3, CP4, RP7, SLO1, SLO3, SLO6 / Published: 09/11/2023
In clinical practice the vast majority of broad complex tachycardias (BCT) will be ventricular in origin.
Ventricular tachycardias (VT) most frequently result from damage to the myocardium secondary to ischaemia, cardiomyopathy or myocarditis, or may result from the effects of drugs such as flecainide or quinidine.
VT is defined as three or more ventricular extra systoles in succession at a rate of more than 120 beats/minute. The term accelerated idioventricular rhythm refers to ventricular rhythms with rates of less than 120 beats/minute.
Learning Bite
Any regular BCT should be assumed to be ventricular in origin.
BCT may be ventricular or supraventricular in origin and the range of arrythmias manifesting as BCT are shown below in Table 1.
Table 1: Types of broad complex tachycardia
| Ventricular origin | Supraventricular origin |
| Monomorphic VT | Tachycardia with aberrant conduction or pre-existing bundle branch block |
| Polymorphic VT | |
| Fascicular tachycardia | |
| Right ventricular outflow tract tachycardia |
Conduction Pathways of the Heart
The clinical presentation, cardinal features and treatment of these arrythmias will be discussed in this module. Figure 1 shows the conduction pathways of the heart and will be referred to when illustrating the origin of various forms of BCT.
Figure 1: The conduction pathways of the heart
(i) Monomorphic ventricular tachycardia
Cardinal Features
Monomorphic refers to a VT where each and every QRS complex is the same shape and size as the next. This form of tachycardia frequently occurs after myocardial infarction when it is a sign of extensive damage.
Cardinal features:
The cardinal features of monomorphic VT are:
- QRS rate is 120-250 beats/min
- QRS rate is regular
- QRS configuration is constant
- QRS configuration is different from that in sinus rhythm
- The QRS complexes are abnormally wide (>0.12s)
Clinical presentation:
As with all tachyarrythmias, symptoms depend upon the ventricular rate and pre-existing cardiovascular state. As the majority of patients with VT have either congenital or acquired heart disease sustained tachycardia often gives rise to symptoms and signs.
These symptoms and signs may be mild (consisting of dizziness or light-headedness), moderate (eg. chest pain or shortness of breath), or severe (with cardiovascular collapse or profound shock). Surprisingly, some patients with severe heart disease may tolerate sustained VT remarkably well and remain asymptomatic.
ECG diagnosis:
Duration and Morphology of the QRS Complex
QRS complexes will all have a similar shape and size with a duration of 0.12 seconds or longer. As a rule, the broader the QRS complex the more likely the rhythm is to be ventricular in origin, particularly if the complexes are over 0.16 seconds.
The pattern of the QRS complexes will usually be like those of right or left bundle branch block. More commonly it is right bundle branch block pattern suggesting that the origin of the arrhythmia is within the left ventricle (See Figures 2 and 3).
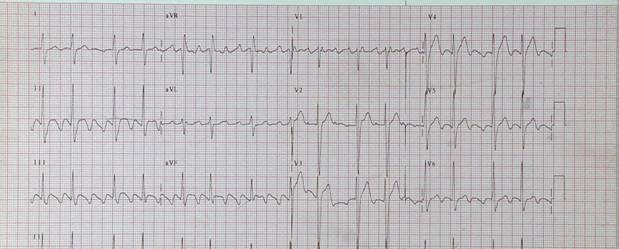
Figure 2: Ventricular tachycardia RBBB pattern
Figure 3: Ventricular tachycardia LBBB pattern
Rate, Rhythm and Frontal Plan Axis
The rate will be 120-250 beats/minute and the rhythm regular. Rates around 150/min or well-tolerated rates above 200 beats/minute should suggest the possibility of a supraventricular origin masquerading as a VT (see below).
Frontal Plane Axis
The axis in a VT is frequently outside the normal range (which is from -30o to +90o ) as the wave of depolarisation frequently moves in the opposite direction to normal.
A wave of depolarisation originating from the apex of the heart and moving to the base may give rise to wildly abnormal axis determinations such as a positive deflection in lead aVR (-210o ).
A monomorphic tachycardia with a positive complex in aVR suggests the axis is bizarre and is very suggestive of a ventricular origin.
Learning Bite
If its up in aVR the axis is bizarre.
Direct or Indirect Evidence of Independent Atrial Activity
It is uncommon to identify evidence of independent atrial activity in a monomorphic ventricular tachycardia, whether this is an occasional P wave or a fusion or captured beat. However, correct identification of these features confirms a diagnosis of VT.
Concordance
Concordance refers to the situation when all the QRS complexes in the chest leads are either positive or negative. The identification of positive or negative concordance suggests the origin of the VT lies in the posterior ventricular wall or anterior ventricular wall respectively.
Learning Bite
Monomorphic ventricular tachycardia is usually regular, has a RBBB pattern and a bizarre axis.
Treatment
In any patient compromised by their monomorphic VT the treatment of choice is DC cardioversion. Signs of instability according to the Resuscitation Council (UK) include reduced conscious level, chest pain, systolic blood pressure of <90 mmHg or heart failure.
Start with a synchronised DC cardioversion at 200 joules (monophasic) or 120-150 joules (biphasic). If unsuccessful repeat the cardioversion up to a maximum of 3 attempts before giving amiodarone. Changing the pad position may be helpful in resistant cases.
Treatment for Patients Who Tolerate Arrhythmia
In patients who are tolerating their arrhythmia, intravenous amiodarone (in a dose of 5mgs/kg up to a maximum of 300mgs) administered over 30 minutes is the treatment of choice. If unsuccessful, DC cardioversion should be considered.
Correction of any underlying abnormalities that might be precipitating the arrhythmia (eg. hypo/hyperkalaemia and hypomagnesaemia) is also required.
(ii) Polymorphic ventricular tachycardia
Polymorphic refers to the fact that the shape and size of each QRS complex varies from the preceding one (see Figure 4)
Figure 4: Polymorphic Ventricular Tachycardia
Polymorphic VT in clinical practice is uncommon and rarely sustained. When polymorphic VT is encountered in the acute setting it is frequently the result of an acute cardiac insult and it rapidly deteriorates into ventricular fibrillation.
Patients with congenital prolonged QT syndromes may present with recurrent episodes of Torsades de pointes.
As with other forms of polymorphic VT, Torsades is not usually sustained but it will recur if the underlying cause is not corrected.
Cardinal Features
- QRS rate is rapid (200 250 beats/min)
- Amplitude of the QRS complexes change in a sinusoidal fashion
- Usually self limiting but may be recurrent
- Between episodes the QT interval is prolonged (see Figure 5)
Learning Bite
Polymorphic VT is uncommon and rarely sustained.
Figure 5: Prolonged QT-interval
Figure 6: Polymorphic Ventricular tachycardia
Treatment
Polymorphic VT that develops in association with an acute coronary syndrome requires immediate DC cardioversion, as it frequently degenerates into ventricular fibrillation. Those patients with Torsades de pointes who are stable require intravenous magnesium and correction of underlying abnormalities (eg. hypokalaemia, hypoxia, etc.) where appropriate.
(iii) Fascicular tachycardia
Fascicular tachycardia (see Figure 7) is uncommon. Patients frequently do not have any underlying structural heart disease and the origin of the tachycardia is the posterior fascicle (or less commonly the anterior fascicle) of the left bundle branch (see Figure 1).
As the wave of depolarisation originates in specialised conducting tissue, the resultant QRS complex is of a relatively short duration (0.11 to 0.14 seconds). Consequently, this arrhythmia is frequently misdiagnosed as a supraventricular tachycardia.
Figure 7: Fascicular Tachycardia
Cardinal Features and Treatment
Cardinal features:
- Right bundle branch block pattern
- Left axis deviation
- QRS duration 0.11 to 0.14 seconds
Treatment:
Fascicular tachycardia should be treated in the same way as monomorphic tachycardia. It is important to identify this arrhythmia correctly so that it is not treated as a supraventricular tachycardia: the administration of verapamil could be dangerous in this setting.
Learning bite
As a fascicular tachycardia originates in specialised conduction tissue, the QRS complexes have a short duration (0.11-0.14 seconds) and as a consequence the arrhythmia may be thought to be supraventricular in origin.
(iv) Right ventricular outflow tachycardia
This tachycardia originates in the right ventricular outflow track which means that the resultant tachycardia has a left bundle branch block type pattern associated with right axis deviation.
Cardinal Features and Treatment
Cardinal features:
- Left bundle branch block
- Right axis deviation
Treatment:
Right ventricular outflow tachycardia usually responds to adenosine, a beta-blocker or a calcium antagonist.
(v) Broad complex tachycardia of supraventricular origin
When faced with a patient with a BCT, the default position should be to assume that the arrhythmia is ventricular in origin until proven otherwise, particularly if the patient is over the age of 35 with a history of ischaemic heart disease or congestive cardiac failure. However, tachycardias with a supraventricular origin can present as a BCT when associated with aberrant conduction or a pre-existing bundle branch block (see Figures 8 and 9).
Cardinal Features and Treatment
Features suggestive of BCT of supraventricular origin:
- Age <35
- Rate =150 beats/minute
- Rate >200 beats/minute and patient asymptomatic
- QRS Duration < 0.14 seconds
- Axis normal
- Absence of independent atrial activity or concordance
Learning Bite
A broad complex tachycardia should be assumed to be ventricular in origin unless there are specific features supporting a supraventricular origin.
Figure 8: Atrial flutter and RBBB (note: rate in excess of 200 beats/min)
Figure 9: Same patient as in Figure 8 following adenosine
Treatment:
Vagal manoeuvres and adenosine (a short acting purine) may be used diagnostically (to help identify BCT which is supraventricular in origin) and therapeutically (to terminate the arrhythmia).
Detailed management of supraventricular tachycardia is discussed in a separate session.
A BCT should be assumed to be ventricular in origin unless there are specific features supporting a supraventricular origin.
(vi) Irregular broad complex tachycardias
Any irregular and sustained broad complex tachycardia should be assumed to be atrial fibrillation with either pre-existing bundle branch block or aberrant conduction (see Figure 10). It is rare for such a rhythm to be ventricular in origin. Although polymorphic VT is irregular, it is rarely sustained.
Atrial fibrillation may occasionally masquerade as polymorphic VT when it is in the presence of pre-excitation. The atrial fibrillation gives rise to an irregular rhythm and the variable conduction down the accessory pathway gives rise to QRS complexes which do change in morphology due to the presence or absence of delta waves giving a similar appearance to Torsades de pointes (see Figure 11).
Learning Bite
Any broad complex tachycardia that is sustained and irregular is most likely to be atrial fibrillation.
Figure 10: Atrial fibrillation and LBBB
Figure 11: Wolff Parkinson White and atrial fibrillation
Treatment:
Once atrial fibrillation is identified as the underlying arrhythmia, it should be treated as such the treatment of atrial fibrillation is discussed in detail in a separate session.
In clinical practice:
- The vast majority of BCT encountered will be VT
- Any broad complex tachycardia that is sustained and irregular is most likely to be atrial fibrillation.
- Any patient with a BCT who is unstable needs urgent synchronised DC cardioversion.
- The cardinal features of monomorphic VT are: wide (>0.12 seconds) and regular QRS complexes with a rate >120 beats/min with a constant morphology which is different from that when the patient is in sinus rhythm.
- The treatment of choice of stable monomorphic VT is intravenous amiodarone.
- The cardinal features of polymorphic VT are: wide and regular QRS complexes with varying amplitude and with a rate between 200 and 250 beats/minute.
- Treatment of Torsades de Point includes intravenous magnesium and correction of underlying electrolyte disturbances.
- The cardinal features of fascicular VT are a right bundle branch block pattern with left axis deviation and a QRS duration of 0.11 0.14 seconds.
- In view of its relatively short QRS complex duration, fascicular tachycardia should not be confused with supraventricular tachycardia.
- The cardinal features of right ventricular outflow tachycardia are left bundle branch block with right axis deviation
- A broad complex tachycardia should be assumed to be ventricular in origin unless there are specific features supporting a supraventricular origin.
- Resuscitation Council UK. Adult Advanced Life Support Guidelines 2021. [Accessed October 2023].
- Tomlinson DR, et al. Intravenous amiodarone for the pharmacological termination of haemodynamically-tolerated sustained ventricular tachycardia: is bolus dose amiodarone an appropriate first-line treatment? Emerg Med J. 2008 Jan;25(1):15-8. [Accessed October 2023].
- Sana M. Al-Khatib. et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Circulation, Vol.138, Issue 13, 25 Sept 2018; Pages e272-e391. [Accessed October 2023].
- Dave J, et al. Torsade de Pointes. Medscape, 2022. [Accessed October 2023].
- Ho KM. Intravenous magnesium for cardiac arrhythmias: jack of all trades. Magnes Res. 2008 Mar;21(1):65-8.
- Joshi S, Wilber DJ. Ablation of idiopathic right ventricular outflow tract tachycardia: current perspectives. J Cardiovasc Electrophysiol. 2005 Sep;16 Suppl 1:S52-8.














10 Comments
I am unable to take the exam. Kindly help
Hi. This is the reference session you are in. If you search for Broad Complex Tachycardias then there should be a Learning Session which pops up allowing you to take the exam
Good reading
Excellent Revision.
Good modules. Useful tips for determining between BCT and SVT, which can frequently be tricky in the clinical setting.
Very useful
this was quite an interesting session, I must say. It clarified things for me
Good revision
Thank you very much!
Very relevant information
very useful and interesting material, thank you for sharing.